Original Article (meta-analysis)
August 2025, 34:2
First online: 18 August 2025
Original Article (meta-analysis)
Outcomes and Management When Using High-sensitivity Versus Conventional Cardiac Troponin in Patients with Acute Chest Pain: A Meta-analysis
John Christopher A. Pilapil,1 Paula Victoria Catherine Y. Cheng-Bromeo,1 Paul Anthony O. Alad,1 Jaime Alfonso M. Aherrera1
Main Author’s Name: John Christopher A. Pilapil
Main Author’s Contact Information:
• Email Address: jcapilapil@gmail.com
• Alternative Email Address: japilapil@up.edu.ph
Institution: Division of Cardiovascular Medicine, Department of Medicine, University of the Philippines – Philippine General Hospital.
Funding: This original investigation is funded solely by the investigators and received no external funding.
Disclosures: The authors of this investigation have no disclosures or conflicts of interest to declare.
ABSTRACT
BACKGROUND
Cardiac troponin (cTn) measurement is pivotal in diagnosing and managing chest pain. High-sensitivity cTn (hs-cTn) assays are slowly supplanting conventional cardiac troponin (c-cTn) use, allowing earlier identification of high-risk patients and diagnosis of myocardial infarction (MI). This improved sensitivity is said to come at the cost of reduced specificity for MI. However, there is a paucity of data regarding the exact impact of this change in patient management and outcomes.
To compare outcomes and management of patients with chest pain when using hs-cTn versus c-cTn assays as part of the diagnostic and therapeutic strategy. METHODS
We conducted a systematic search of studies in all languages across various databases. Inclusion criteria for studies were (1) observational or randomized trials, (2) included adult patients presenting with chest pain, (3) use of hs-cTn or c-cTn in diagnosis, (3) reported data on any of the pre-defined outcomes. The primary outcome was all-cause mortality and secondary outcomes were major adverse cardiovascular events (MACE), MI following index admission, coronary angiography, and revascularization. Study quality was appraised using the Cochrane Tool for Assessing Risk of Bias for randomized trials and the Newcastle-Ottawa Quality Assessment scale for observational studies. Outcomes were analyzed using Review Manager (RevMan) 5.3, employing Mantel-Haenszel analysis of random effects to compute for relative risk and odds ratio. RESULTS
Pooled analysis from 5 studies showed that among patients with chest pain, those for whom hs-cTn over c-cTn was used had no difference in all-cause mortality (RR 1.01, 95% CI 0.92-1.12, p=0.82, I2=0%), a significant decrease in MI (RR 0.74, 95% CI 0.63-0.87, p=0.0003) and a trend towards increase in MACE (RR 1.08, 95% CI 1.00-1.16, p=0.04, I2=0%). They were more likely to undergo coronary angiogram (OR 1.52, 95% CI 1.02-2.28, p=0.04) and revascularization (OR 1.34, 95% CI 1.03-1.75, p=0.03). CONCLUSION
Use of hs-cTn over conventional cTn led to higher rates of coronary angiography and revascularization, with no reduction in all-cause mortality and no significant MACE reduction.
CONDENSED ABSTRACT
Cardiac troponin (cTn) measurement is pivotal in diagnosing and managing chest pain. High-sensitivity cTn (hs-cTn) assays are supplanting conventional cardiac troponin (c-cTn) use, allowing earlier identification of high-risk patients and diagnosis of myocardial infarction (MI). There is a paucity of data regarding the exact clinical impact of this change. We conducted a systematic search of studies comparing outcomes and management of patients with acute chest pain when using hs-cTn vs. c-cTn. Pooled analysis showed the use of hs-cTn vs. c-cTn led to higher rates of coronary angiography and revascularization, with no reduction in all-cause mortality and no significant MACE reduction.
KeywordsCardiac Troponin, High Sensitivity, Acute Chest Pain, Acute Coronary Syndrome
Abbreviations
- Ischemic heart disease (IHD)
- Coronary artery disease (CAD)
- Acute coronary syndrome (ACS)
- MI (Myocardial infarction)
- Cardiac troponin (cTn: T or I; cTnT or cTnI)
- Conventional cTn (c-cTn)
- High-sensitivity cTn (hs-cTn)
I. INTRODUCTION
Acute Chest Pain
Acute chest pain remains to be one of the most common complaints for seeking care in the emergency department (ED). Next to injuries, chest pain is the second most common complaint in the United States – accounting for over 7 million or 4.7% of all annual ED visits and almost 10% of approximately 100 million non-traumatic visits.1, 2 The lifetime prevalence of chest pain is estimated at 20-40%, with more women than men experiencing the symptom. More than 60% of patients at the ED with this presentation are admitted for further evaluation.3, 4
Pathologies involving the heart, vasculature, lungs, pleura, mediastinal structures, gastrointestinal tract, musculoskeletal system, and nervous system may all present with chest discomfort.5 Although the determined cause of patients at the ED with acute chest pain is typically non-cardiac, ischemic heart disease (IHD) still represents 31% of all etiologies and is the most common serious, life-threatening cause.6 Chest pain, in turn, remains to be the most common symptom of the entire spectrum of coronary artery disease (CAD) – both acute and chronic disease – in men and women.7 Of all patients presenting to the ED with chest pain, an estimated 5-15% will have acute coronary syndrome (ACS).
Thus, chest pain continues to prove itself as a diagnostic challenge, requiring thorough clinical evaluation and prudent, prompt use of diagnostics in both the outpatient and ED setting. Differentiating patients with ACS and CAD or other life-threatening conditions – cardiac and non-cardiac alike – from those with non-cardiovascular, non-life-threatening chest pain is of paramount importance to the attending clinician.
Cardiac Troponin Assays: High Sensitivity vs. Conventional
Patients presenting with acute chest pain suspected to have ACS necessitate measurement of biomarkers for myocardial injury.8, 9, 10, 11 Cardiac troponin (cTn: T or I; cTnT or cTnI) is the preferred biomarker. cTnI and cTnT are cardiac regulatory proteins involved in calcium-mediated actin and myosin interaction.12 Since they are products of genes expressed almost exclusively by cardiac tissue, cTn’s are potentially specific cardiac isoforms and essentially unique to the heart.13-14 In their clinical use, both cTnT and cTnI have shown equal utility and diagnostic capability.15 The once popular creatinine kinase MB isoenzyme (CK-MB) is no longer recommended due to its lack of sensitivity and specificity.8-11, 12-14
Assays for cTn measurement are done using enzyme-linked immunosorbent testing techniques and are available with varying sensitivities to levels of the biomarker of interest.16 The limit of detection is defined as the lowest, detectable cTn concentration that is accurately measured in a sample containing low cTn concentration.17-18 Compared with the older conventional cTn (c-cTn) assays, high-sensitivity cTn (hs-cTn) assays have the distinction of being able to detect cTn values above the limit of detection in at least 50% of normal individuals.19
The advent of modern hs-cTn assays enable earlier detection of MI, essentially shifting the conventions for workup of chest pain by allowing early “rule-out” strategies.20-23 Due to their greater precision at the lower range of measurable troponin level, hs-cTn as opposed to c-cTn assays allow: (1) determination if the cTn in a blood sample is elevated or above the upper limit of normal, and moreover, (2) reliable detection of absolute changes in samples obtained serially at presentation and hours later.21-27 The more sensitive examination by hs-cTn assays not only of absolute cTn levels, but dynamic changes as well has thus shortened the time interval to the next measurement from a historical practice of 6-12 or more hours to 1-2 hours. All of this while still achieving good negative predictive values of ≥ 99%.8-9, 24-27 Such changes in clinical algorithms and strategies have likewise facilitated discharging patients on the basis of a single cTn value at presentation with reasonable safety.9, 11, 28
The preferential use of hs-cTn assays for biomarker measurement has likewise allowed for the detection of potentially fatal and intervenable disease in a broader range of patients. The heightened sensitivity for detection of ACS, however, also includes patients with other causes of cTn elevation.28-30 Reasons of elevation of cTn values due to myocardial injury appear to be all-encompassing and may include injury due to myocardial ischemia by virtue of CAD and atherosclerotic plaque disruption with thrombosis, myocardial ischemia due to oxygen supply/demand imbalance, and other “miscellaneous” causes of myocardial injury – such as non-CAD cardiac conditions and various systemic diseases.20 A previous collaborative meta-analysis has suggested that hs-cTn assays improve early sensitivity and negative predictive value for the diagnosis of ACS and acute MI, but at the expense of specificity and positive predictive value.30
Importance and Significance of the Study
Hs-cTn assays are now preferred over c-cTn assays, as recommended by the Fourth Universal Definition of Myocardial Infarction. Here, myocardial injury is defined as the detection of an elevated cTn value above the 99th percentile upper reference limit. Furthermore, the presence of a rise and/or fall of cTn values is said to be indicative that the injury is acute.20 The recommendation for using hs-cTn over c-cTn assays in consistent in practically all guidelines detailing the diagnosis and management of myocardial infarction (MI).8-11, 20 With this, the use of hs-cTn continues to replace c-cTn in the approach to patients presenting with acute chest pain at the ED.
As discussed, the advent of hs-cTn assays has allowed earlier identification of high-risk patients and diagnosis of ACS among the general population presenting with chest pain. This improved sensitivity, however, seemingly comes at the cost of a reduced specificity for MI. While hs-cTn has slowly supplanted c-cTn in practice, there is a paucity of data as to the exact impact of this change in patient management and outcomes. Prior data suggests that hs-cTn use over c-cTn may improve prognosis, but data is wanting to definitively confirm this.31
The necessity of looking into the particularities of hs-cTn vs. c-cTn use in patients with chest pain is perhaps made all the important by the fact that in recent past, numerous advances and trials have yielded paradigm shifts in the way we approach patients with chest pain and subsequently manage those confirmed to have ACS – whether via conservative/medical or invasive strategies. Our study is the first of its kind to consolidate data on the management and outcomes of hs-cTn vs. c-cTn use in adult patients presenting at the ED with chest pain.
II. METHODS
Literature Search
We conducted a systematic search of studies that compared outcomes and management of patients with chest pain using hs-cTn versus conventional cTn. Meta-analyses, systematic reviews, randomized controlled trials, cohort studies, and observational studies on the following electronic databases were eligible for inclusion: PubMed, Cochrane Library, MEDLINE, EMBASE, WHO Network of Collaborating Clinical Trial Registers, ScienceDirect, and ClinicalTrials.gov. The following free text and MeSH terms were used in our search strategy: high sensitivity cardiac troponin, conventional cardiac troponin, chest pain, chest discomfort, angina, acute coronary syndrome, and myocardial infarction. Search for available literature PubMed was further refined by using high-sensitivity method filters to sift out applicable study designs. Retrieved articles’ reference lists were likewise examined to identify additional potential studies for inclusion. We attempted to contact study authors and known experts in the field to search for additional published and unpublished data alike.
Study Inclusion
Two authors independently assessed the retrieved articles to determine those for inclusion in this meta-analysis. We determined the following pre-specified inclusion criteria for studies: (1) adult patients ≥ 19 years old presenting with chest pain or discomfort, (2) use of hs-cTn vs. c-cTn, (3) outcomes of all-cause mortality, major adverse cardiac events, myocardial infarction, (4) performance of coronary angiography and revascularization.
Data Collection and Analysis
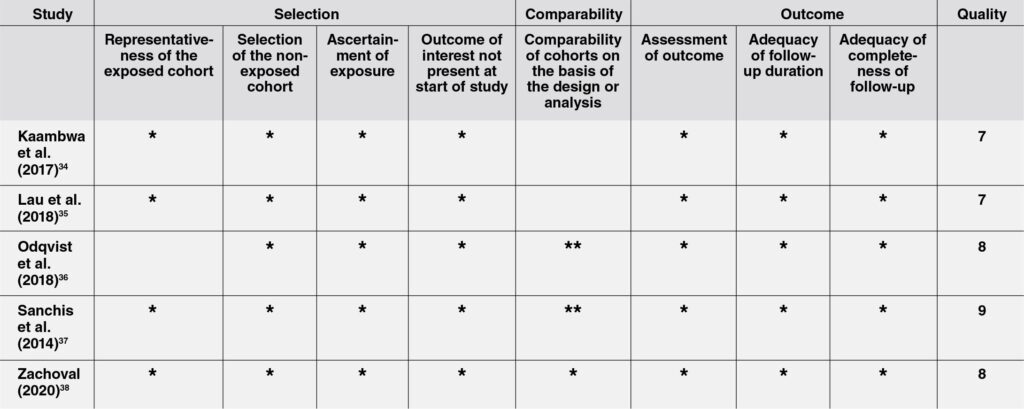
Assessment of Risk of Bias in Included Studies
Two reviewers independently assessed the validity and risk of bias of retrieved articles. The Newcastle-Ottawa Quality Assessment Form was utilized for cohort studies and case control studies.32 Articles were determined to be of good, fair, or poor quality. Disputes and disagreements with regard to the article appraisal was settled by discussion and consensus of the reviewers with a third author who served as arbiter.
Data Extraction and Management
Two reviewers independently extracted the data using a uniform data extraction form. The following data were extracted from each study: all-cause mortality, major adverse cardiovascular events, myocardial infarction following index admission, performance of coronary angiography, and revascularization.
Measures of Treatment Effect and Heterogeneity
Data was analyzed using Review Manager 5, utilizing the Mantel-Haenszel test statistical method and random effects model. Clinical outcomes were calculated for their relative risks, while management strategies employed were calculated for their odds ratios. Data from each trial included was synthesized and combined for cases deemed appropriate. A 95% confidence interval was also presented with each result. Heterogeneity of studies was assessed by analyzing the study characteristics, and similarities or differences between participants, interventions, results, and methodologies. Heterogeneity was determined using the I2 and chi-square measures of heterogeneity, setting a value of more than or equal to 50% I2 and less than or equal to 10% p-value to indicate statistically significant heterogeneity.
Data Analysis and Synthesis
Data analysis and synthesis was done through the Review Manager 5 software. Relative risks, risk ratios, and odds ratios of dichotomous variables were calculated using the random effects model.
III. RESULTS
INCLUDED AND EXCLUDED STUDIES
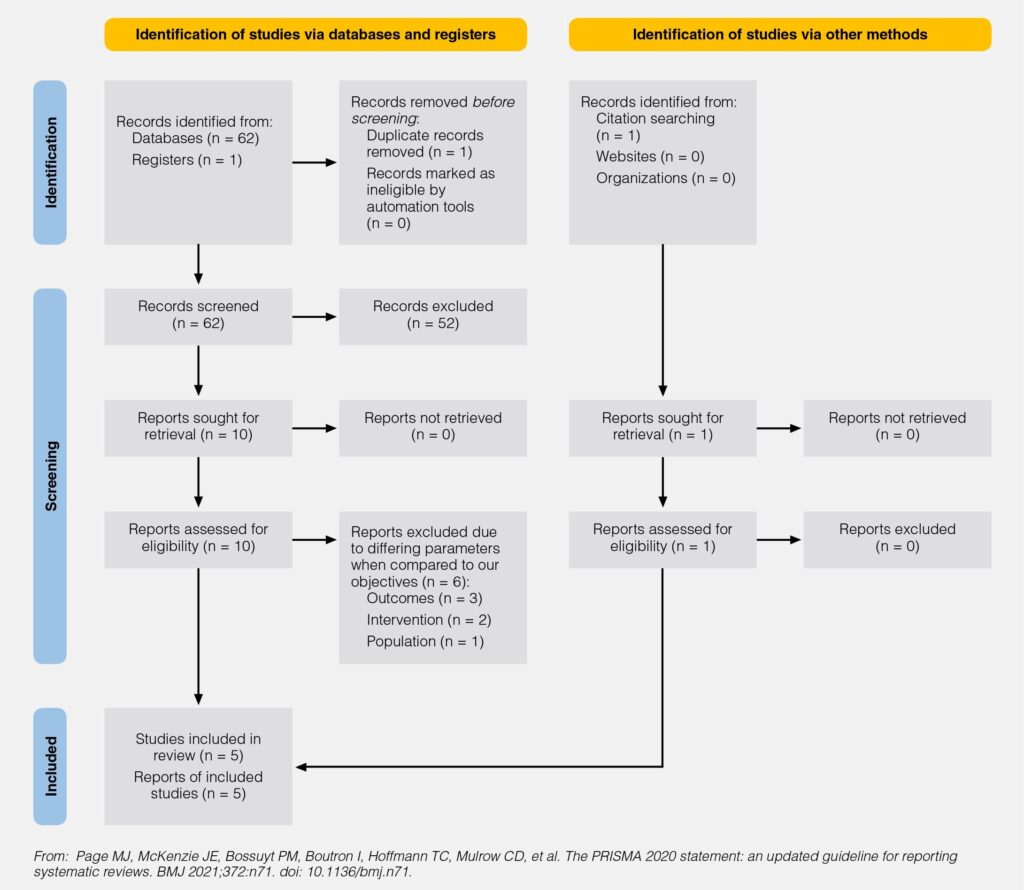
Initial search and identification of studies yielded 62 non-duplicate records from the various databases and registries listed in this study’s methods section, which were then screened by the reviewers using the set selection criteria for studies. A
total of 52 articles were excluded after screening the studies’ titles and abstracts. 10 articles were retrieved for full-text review. Among these, 6 were further excluded due to non-compatibility with this study’s selection criteria – three of the articles did not include any of our desired and pre-specified outcomes, two articles had different investigated interventions, and one article analyzed a different population compared to our research objectives. Among the remaining 4 articles, another 1 was identified via citation searching and deemed eligible. A total of 5 studies were included in the final list of studies for the meta-analysis. The PRISMA workflow chart33 showing article and study
identification, screening, inclusion, and exclusion may be found in Supplemental Appendix A.
STUDY CHARACTERISTICS AND QUALITY
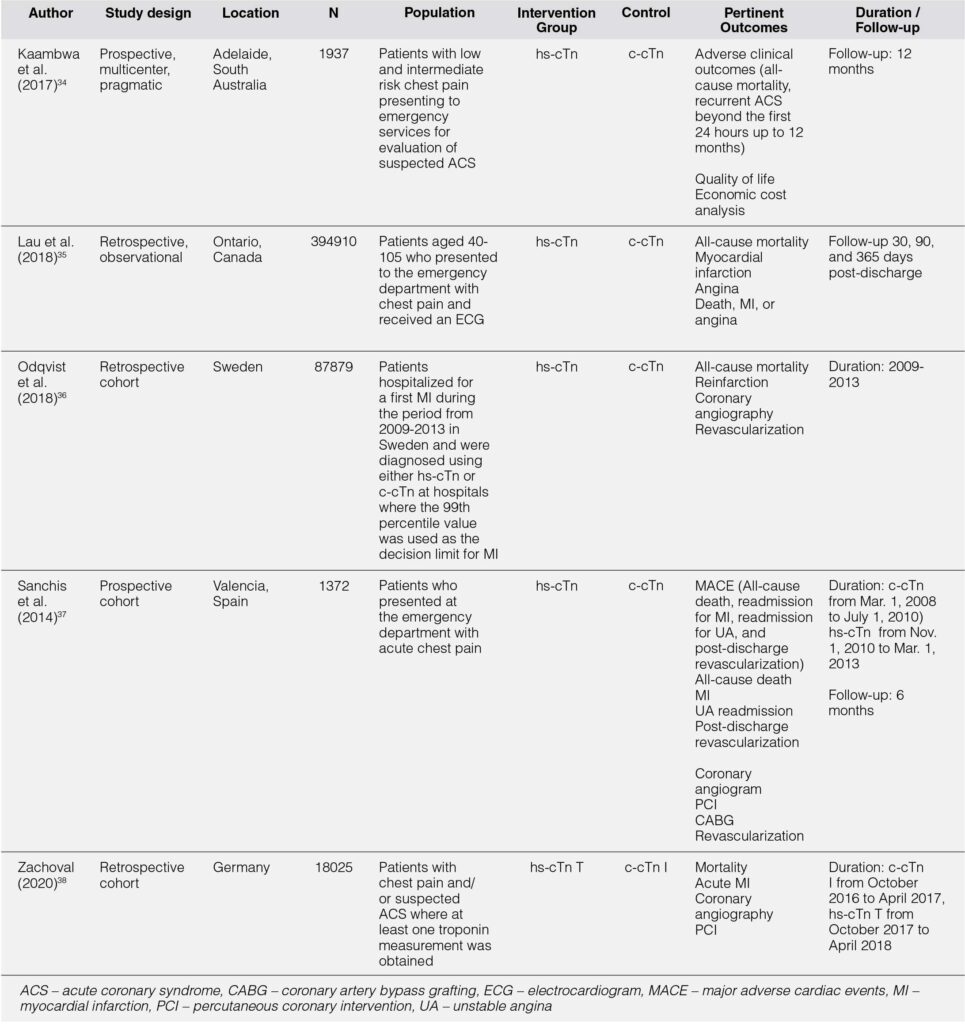
Five retrieved studies (n = 504,123) met our inclusion criteria and were included in the final analysis.34-38 All of the studies were observational in design. Two of the retrieved articles utilized a prospective design, while the other three were retrospective in nature. Individual study populations ranged from 3,492 to 394,910. No randomized trials were found by our search for articles. The populations involved for four of the studies were adult patients presenting to the emergency department with chest pain and suspected ACS. One study looked at adult presents presenting with chest pain who were subsequently diagnosed for the first time with ACS.36 All of the included studies reported at least one of our specified outcomes of interest. Follow-up of patients ranged from as short as 30 days to as long as nearly 3 years. All of the studies were of good quality by the Newcastle-Ottawa Scale. Table 1 summarizes the characteristics of included studies. The details of risk of bias assessment may be found in Supplemental Appendix B.
OUTCOMES
Primary Outcome
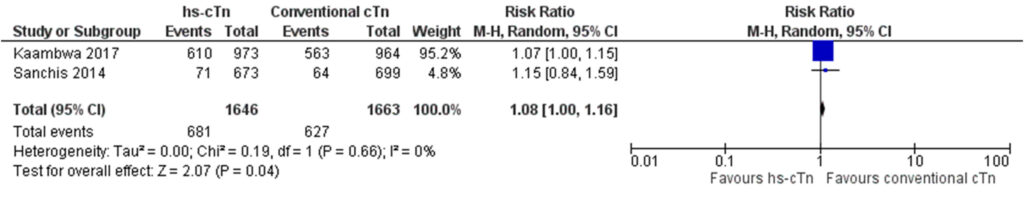
Four studies (n = 502,166) were included in the initial analysis (Fig. 1). Pooled data showed that the use of hs-cTn over c-cTn had no effect on all-cause mortality (RR 0.94, 95% CI 0.76-1.16, p = 0.54). Results, however, were with significant heterogeneity (I2 = 90%). The study authors identified the study by Odqvist et al36 to be a contributor to the noted heterogeneity. Having included patients already diagnosed with myocardial infarction renders their study population already of high risk at the onset. The effect of using hs-cTn that would lead to earlier and perhaps more aggressive interventions, therefore, was postulated to contribute to heterogeneity by skewing benefit towards the use of hs-cTn.
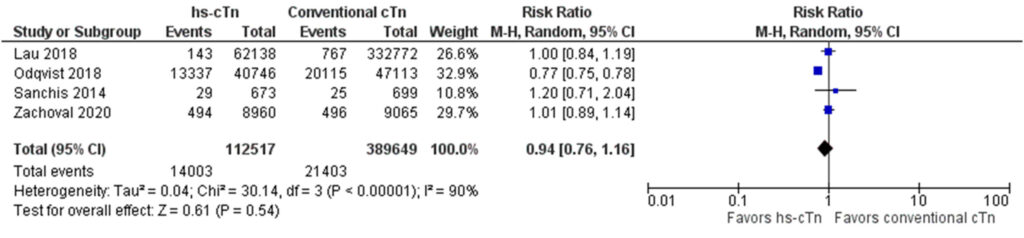
An analysis adjusting for the identified source of heterogeneity (Fig. 2) was thus carried out, identifying the study of Odqvist et al due to its population being of higher risk for cardiovascular events compared to the others. From this, three studies (n = 414,307) were included in the final analysis. This revealed that, indeed, the use of hs-cTn over c-cTn did not lead to differences in all-cause mortality (RR 1.01, 95% CI 0.92-1.12, p=0.82).
Secondary Outcomes
Secondary Clinical Outcomes
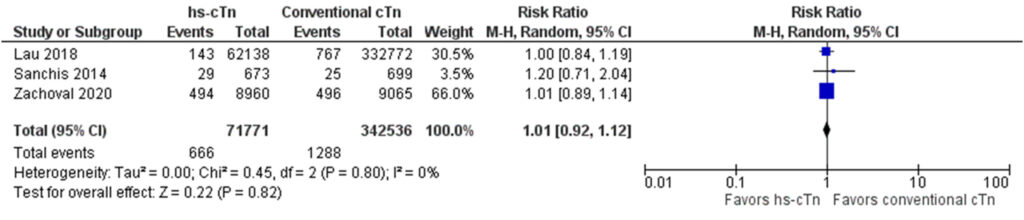
Major Adverse Cardiovascular Events (MACE)
Two studies (n = 3,309) reporting on MACE were included in the analysis (Fig. 3). Results showed that the use of hs-cTn as opposed to c-cTn did not lead to a significant reduction in MACE, without significant heterogeneity (RR 1.08, 95% CI 1.00-1.16, p=0.04, I2=0%). They even noted a signal towards harm that would appear to favor using c-cTn.
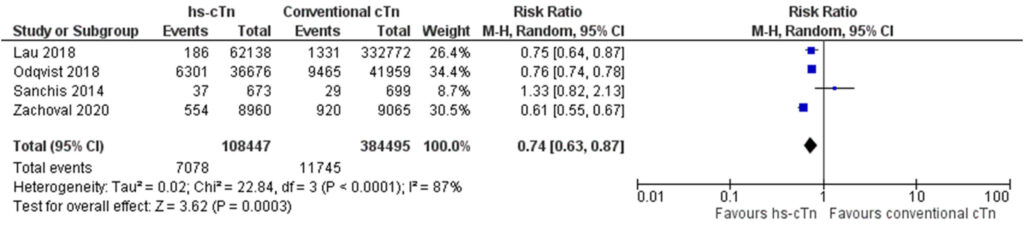
Myocardial Infarction on Follow-up
A total of 4 studies (n = 492,942) were included in this analysis (Fig. 4), which showed that there was an overall statistically significant decrease in the incidence of myocardial infarction on subsequent follow-ups of patients for whom hs-cTn was used instead of c-cTn as part of the diagnostic strategy (RR 0.74, 95% CI 0.63-0.87, p=0.0003), but with significant heterogeneity of these results (I2=87%).
Management of Patients
Performance of Coronary Angiogram
With three studies (n = 107,276) included in the final analysis (Fig. 5), results reveal that there was a statistically significant increase in the performance of coronary angiogram among patients for whom hs-cTn was used over c-cTn (OR 1.52, 95% CI 1.02-2.28, p=0.04). Results were with heterogeneity (I2=98%).

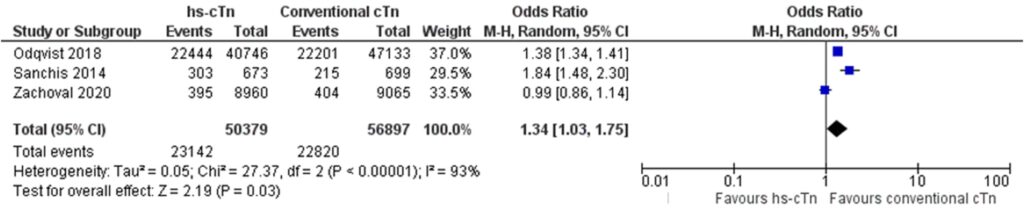
Performance of Revascularization
Three studies (n = 107,276) were included in the analysis
(Fig. 6). There was a statistically significant increase in
revascularization among patients for whom hs-cTn was used
instead of c-cTn (OR 1.34, 95% CI 1.03-1.75, p=0.03), but with heterogeneous results (I2=93%).
IV. DISCUSSION
Our meta-analysis, which included 5 cohort studies involving 504,123 patients, is the first to consolidate and analyze data pertaining to the management and outcomes of patients presenting to the ED with chest pain when using hs-cTn vs. c-cTn as part of the diagnostic strategy and patient approach. Our analysis shows the following results that may be highlighted into two points. First, the use of hs-cTn when compared with c-cTn in these patients led to more interventions being performed, with higher rates of coronary angiography and revascularization. Secondly, with this increased performance of diagnostic and therapeutic procedures, there was a significant decrease in MI on follow-up, but no reduction in all-cause mortality and even a signal towards increased major cardiac events.
Effects on Patient Management
This study shows that using hs-cTn over c-cTn assays led to statistically significant increased odds for the performance of coronary angiogram (OR 1.52, 95% CI 1.02-2.28, p=0.04). There was likewise an increase in the odds of revascularization (OR 1.34, 95% CI 1.03-1.75, p=0.03) – whether via coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI), inclusive of balloon angioplasty with or without stent implantation.
A possible explanation to this observed phenomenon is that an early invasive approach (via coronary angiogram with the intent to revascularize diseased vessels) is recommended for patients with acute coronary syndrome diagnosed to have myocardial infarction and also in those with a significant rise and/or fall in cTn values on serial measurement.8-11 As we have detailed in our review of literature, hs-cTn unveils cTn elevation in some patients who otherwise would initially pass undetected using a conventional assay.18, 19, 29, 30 Indeed, in an early study analyzing the effects of shift from c-cTn to hs-cTn use in patients at the ED with chest pain, there was a noted increase in prevalence of MI from 18% to 22%.39 Initial concern was hence expressed that the introduction of hs-cTn assays would be followed by a concomitant increase in MI’s.36 Subsequent studies, however, have had conflicting and ambivalent results. While some did not any change in reported MI’s with the use of hs-cTn assays over c-cTn assays,40 others demonstrated higher MI prevalence36, 37, 41 and in some studies, even a decrease in the number of MI’s reported.42 It is important to note that because the kinetics of troponin rise and fall are multifactorial, there is still no definitive criteria for what cTn change or “delta” is significant.43 Since part of the diagnosis of MI is established by the pattern of rise and fall in cTn and not just cTn elevation alone, this may have contributed to the differences in the above observations with regard to the effect of hs-cTn use on MI prevalence.
Apart from the diagnosis of MI and demonstrable rise and/or fall in cTns, early performance (within 24 hours of diagnosis) of coronary angiogram is also recommended patients deemed high risk8-11 via risk calculators such as the GRACE score for ACS44 and TIMI score for non-ST elevation MI.45 As these risk calculators frequently include elevated cTn’s as predictors that elevate the risk for events, it is possible that the more sensitive detection of even low levels of cTn by high sensitivity assays lead to higher risk scores for ACS patients overall, although there have yet to be any studies looking into this.
Significant heterogeneity was seen in our pooled analysis of results for both coronary angiogram and revascularization performance. Potential sources of this may be the wide range in time period in which the included studies were performed. These studies were likewise done across different countries. It may be possible that the recommendations and practices for ACS significantly differed across different eras, locales, and per-hospital or institution predicaments – thus leading to heterogeneity in results for both patient management odds and outcome risks.
Effects on Patient Outcomes
Our results show that among patients with chest pain for whom hs-cTn over c-cTn assay was used, there was no difference in all-cause mortality after adjusting for sources of heterogeneity (RR 1.01, 95% CI 0.92-1.12, p=0.82, I2=0%). Meanwhile, a significant decrease in MI was observed (RR 0.74, 95% CI 0.63-0.87, p=0.0003, I2=87%) and quite strikingly, there was a trend towards increase in MACE (RR 1.08, 95% CI 1.00-1.16, p=0.04, I2=0%).
Our results showing a decrease in risk of MI on follow-up are seemingly consistent with available evidence that, particularly among symptomatic CAD patients, revascularization is beneficial in relieving symptoms and potentially reducing the risk of future MI.46-47 The noted signal for harm and higher MACE could potentially be correlated with our findings of increased performance of coronary angiography and revascularization. PCI and CABG have concomitant risk for major complications – such as death, MI, or stroke – and minor complications – such as transient ischemic attacks, vascular complications, contrast-induced nephropathy, and angiographic complications.48-50 In theory, higher performance of procedures would yield higher prevalence of its possible complications. This might have been the case we see for our results on MACE.
Ultimately, there was no reduction in all-cause mortality when using hs-cTn over c-cTn. In light of increased performance of angiography and revascularization and reduced MI but a trend towards increased MACE, it is important to emphasize the necessity to weigh and carefully analyze the implications of preference for hs-cTn assay use in approaching with chest pain. Benefits, risks, and costs must be taken into consideration. A prior study in Australia already demonstrated that hs-cTn use had a tendency for higher health costs. In spite of fewer adverse clinical outcomes, the cost effectiveness of hs-cTn over c-cTn use was high at $108,552 per adverse clinical outcome avoided.34 Increase in resource use leading to increased costs and higher exposure of patients to potential complications – even with the possibility for certain benefits – is a concern that must not go unnoticed.
As previously mentioned, there is a paucity of data with regard to comparing how using hs-cTn vs. c-cTn may affect how physicians decide to manage acute MI patients (e.g. to proceed with invasive coronary angiography and/or revascularization or not) and ultimately, what outcomes are achieved – are mortality, MACE, and other endpoints reduced or are they just the same? This may be due to the fact that pre-existing studies have mainly focused on the diagnostic capability, sensitivity, and specificity of hs-cTn vs. c-cTn in myocardial infarction. The results of this meta-analysis, therefore, emphasize the need for more endeavors investigating the impact of using hs-cTn in clinical practice. Therefore, it is our recommendation that more carefully and well-designed randomized studies should be carried out, looking into the implications on patient management, resource use, and outcomes of using hs-cTn over c-cTn.
Study Limitations
This investigation included only articles published in English. Furthermore, there were no randomized trials found and all studies included were only observational in design. Some of the included articles were followed-up patients who were managed before more recent changes in diagnostic and therapeutic interventions for acute MI as well.
V. CONCLUSION
Among patients presenting with chest pain, the use of hs-cTn when compared with c-cTn led to higher rates of performing coronary angiography and revascularization. While there was a significant decrease in MI on follow-up, there as no reduction in all-cause mortality and even a signal towards increased MACE.
REFERENCES
1. Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines. Clinical Practice Guidelines We Can Trust. Washington, DC: National Academies Press. 2011.
2. Institute of Medicine (US) Committee on Standards for Systematic Reviews of Comparative Effectiveness Research. Finding What Works in Health Care: Standards for Systematic Reviews. Washington, DC: National Academies Press. 2011. CrossRef Pubmed
3. Lichtman JH, Leifheit EC, Safdar B, et al. Sex Differences in the Presentation and Perception of Symptoms Among Young Patients With Myocardial Infarction: Evidence from the VIRGO Study (Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients). Circulation. 2018;137(8):781-790. doi:10.1161/CIRCULATIONAHA.117.031650 CrossRef Pubmed
4. Bösner S, Becker A, Haasenritter J, et al. Chest pain in primary care: epidemiology and pre-work-up probabilities. Eur J Gen Pract. 2009;15(3):141-146. doi:10.3109/13814780903329528 CrossRef Pubmed
5. Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144(22):e368-e454. doi:10.1161/CIR.0000000000001030 CrossRef Pubmed
6. Fruergaard P, Launbjerg J, Hesse B, et al. The diagnoses of patients admitted with acute chest pain but without myocardial infarction. Eur Heart J. 1996;17(7):1028-1034. doi:10.1093/oxfordjournals.eurheartj.a014998 CrossRef Pubmed
7. Swap CJ, Nagurney JT. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes [published correction appears in JAMA. 2006 May 17;295(19):2250]. JAMA. 2005;294(20):2623-2629. doi:10.1001/jama.294.20.2623 CrossRef
8. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines [published correction appears in J Am Coll Cardiol. 2014 Dec 23;64(24):2713-4. Dosage error in article text]. J Am Coll Cardiol. 2014;64(24):e139-e228. doi:10.1016/j.jacc.2014.09.017 CrossRef Pubmed
9. Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation [published correction appears in Eur Heart J. 2021 May 14;42(19):1908] [published correction appears in Eur Heart J. 2021 May 14;42(19):1925] [published correction appears in Eur Heart J. 2021 May 13;:]. Eur Heart J. 2021;42(14):1289-1367. doi:10.1093/eurheartj/ehaa575 CrossRef Pubmed
10. O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78-e140. doi:10.1016/j.jacc.2012.11.019 CrossRef Pubmed
11. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177. doi:10.1093/eurheartj/ehx393 CrossRef Pubmed
12. Adams JE 3rd, Abendschein DR, Jaffe AS. Biochemical markers of myocardial injury. Is MB creatine kinase the choice for the 1990s?. Circulation. 1993;88(2):750-763. doi:10.1161/01.cir.88.2.750 CrossRef Pubmed
13. Adams JE 3rd, Bodor GS, Dávila-Román VG, et al. Cardiac troponin I. A marker with high specificity for cardiac injury. Circulation. 1993;88(1):101-106. doi:10.1161/01.cir.88.1.101 CrossRef Pubmed
14. Bodor GS, Porterfield D, Voss EM, Smith S, Apple FS. Cardiac troponin-I is not expressed in fetal and healthy or diseased adult human skeletal muscle tissue. Clin Chem. 1995;41(12 Pt 1):1710-1715. Pubmed
15. Sandoval Y, Herzog CA, Love SA, et al. Prognostic Value of Serial Changes in High-Sensitivity Cardiac Troponin I and T over 3 Months Using Reference Change Values in Hemodialysis Patients. Clin Chem. 2016;62(4):631-638. doi:10.1373/clinchem.2015.251835 CrossRef Pubmed
16. Wu AHB, Christenson RH, Greene DN, et al. Clinical Laboratory Practice Recommendations for the Use of Cardiac Troponin in Acute Coronary Syndrome: Expert Opinion from the Academy of the American Association for Clinical Chemistry and the Task Force on Clinical Applications of Cardiac Bio-Markers of the International Federation of Clinical Chemistry and Laboratory Medicine. Clin Chem. 2018;64(4):645-655. doi:10.1373/clinchem.2017.277186 CrossRef Pubmed
17. Pickering JW, Than MP, Cullen L, et al. Rapid Rule-out of Acute Myocardial Infarction With a Single High-Sensitivity Cardiac Troponin T Measurement Below the Limit of Detection: A Collaborative Meta-analysis [published correction appears in Ann Intern Med. 2017 Oct 3;167(7):528]. Ann Intern Med. 2017;166(10):715-724. doi:10.7326/M16-2562 CrossRef Pubmed
18. Sandoval Y, Smith SW, Apple FS. Present and Future of Cardiac Troponin in Clinical Practice: A Paradigm Shift to High-Sensitivity Assays. Am J Med. 2016;129(4):354-365. doi:10.1016/j.amjmed.2015.12.005 CrossRef Pubmed
19. Apple FS. A new season for cardiac troponin assays: it’s time to keep a scorecard. Clin Chem. 2009;55(7):1303-1306. doi:10.1373/clinchem.2009.128363 CrossRef Pubmed
20. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol. 2018;72(18):2231-2264. doi:10.1016/j.jacc.2018.08.1038 CrossRef Pubmed
21. Morrow DA. Evidence-Based Algorithms Using High-Sensitivity Cardiac Troponin in the Emergency Department. JAMA Cardiol. 2016;1(4):379-381. doi:10.1001/jamacardio.2016.1205 CrossRef Pubmed
22. Mueller C, Giannitsis E, Möckel M, et al. Rapid rule out of acute myocardial infarction: novel biomarker-based strategies. Eur Heart J Acute Cardiovasc Care. 2017;6(3):218-222. doi:10.1177/2048872616653229 CrossRef Pubmed
23. Mueller C, Giannitsis E, Christ M, et al. Multicenter Evaluation of a 0-Hour/1-Hour Algorithm in the Diagnosis of Myocardial Infarction With High-Sensitivity Cardiac Troponin T. Ann Emerg Med. 2016;68(1):76-87.e4. doi:10.1016/j.annemergmed.2015.11.013 CrossRef Pubmed
24. Peacock WF, Baumann BM, Bruton D, et al. Efficacy of High-Sensitivity Troponin T in Identifying Very-Low-Risk Patients With Possible Acute Coronary Syndrome [published correction appears in JAMA Cardiol. 2018 Sep 1;3(9):898]. JAMA Cardiol. 2018;3(2):104-111. doi:10.1001/jamacardio.2017.4625 CrossRef Pubmed
25. Pickering JW, Than MP, Cullen L, et al. Rapid rule-out of acute myocardial infarction with a single high-sensitivity cardiac troponin T measurement below the limit of detection: a collaborative meta-analysis. Ann Intern Med. 2017;166(10):715–724. CrossRef Pubmed
26. Reichlin T, Twerenbold R, Wildi K, et al. Prospective validation of a 1-hour algorithm to rule-out and rule-in acute myocardial infarction using a high-sensitivity cardiac troponin T assay. CMAJ (Can Med Assoc J). 2015;187(8):E243–E252. CrossRef Pubmed
27. Rottger E, de Vries-Spithoven S, Reitsma JB, et al. Safety of a 1-hour rule out high-sensitive tro¬ponin T protocol in patients with chest pain at the emergency department. Crit Pathw Cardiol. 2017;16(4):129–134. CrossRef Pubmed
28. Sanchis J, Valero E, García Blas S, et al. Undetectable high-sensitivity troponin in combination with clinical assessment for risk stratification of patients with chest pain and normal troponin at hospital arrival. Eur Heart J Acute Cardiovasc Care. 2020;9(6):567-575. doi:10.1177/2048872620907539 CrossRef Pubmed
29. Hammerer-Lercher A, Ploner T, Neururer S, et al. High-sensitivity cardiac troponin T compared with standard troponin T testing on emergency department admission: how much does it add in everyday clinical practice?. J Am Heart Assoc. 2013;2(3):e000204. Published 2013 Jun 4. doi:10.1161/ JAHA.113.000204 CrossRef Pubmed
30. Lipinski MJ, Baker NC, Escárcega RO, et al. Comparison of conventional and high-sensitivity troponin in patients with chest pain: a collaborative meta-analysis. Am Heart J. 2015;169(1):6-16.e6. doi:10.1016/j.ahj.2014.10.007 CrossRef Pubmed
31. Mills NL, Churchhouse A, Lee KK, et al. Implementation of a sensitive troponin I assay and risk of recurrent myocardial infarction and death in patients with suspected acute coronary syndrome. J Am Heart Assoc. 2011;305:1210–16. CrossRef Pubmed
32. Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Accessed November 7, 2022. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
33. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. Published 2021 Mar 29. doi:10.1136/bmj.n71 CrossRef Pubmed
34. Kaambwa B, Ratcliffe J, Horsfall M, et al. Cost effectiveness of highsensitivity troponin compared to conventional troponin among patients presenting with undifferentiated chest pain: A trial based analysis. Int J Cardiol. 2017;238:144-150. doi:10.1016/j.ijcard.2017.02.141 CrossRef Pubmed
35. Lau G, Koh M, Armstrong D, Udell J, Wang X, Sivaswamy A. Ko D. High-sensitivity vs. conventional troponin assays in the emergency department: post-discharge outcomes in real world practice. Can J Cardiol. 2018;34:S51-S52. CrossRef
36. Odqvist M, Andersson PO, Tygesen H, Eggers KM, Holzmann MJ. High-Sensitivity Troponins and Outcomes After Myocardial Infarction. J Am Coll Cardiol. 2018;71(23):2616-2624. doi:10.1016/j.jacc.2018.03.515 CrossRef Pubmed
37. Sanchis J, García-Blas S, Mainar L, et al. High-sensitivity versus conventional troponin for management and prognosis assessment of patients with acute chest pain. Heart. 2014;100(20):1591-1596. doi:10.1136/heartjnl-2013-305440 CrossRef Pubmed
38. Zachoval CF, Dolscheid-Pommerich R, Graeff I, et al. High-Sensitivity Troponin T Testing: Consequences on Daily Clinical Practice and Effects on Diagnosis of Myocardial Infarction. J Clin Med. 2020;9(3):775. Published 2020 Mar 12. doi:10.3390/jcm9030775 CrossRef Pubmed
39. Reichlin T, Twerenbold R, Reiter M, et al. Introduction of high-sensitivity troponin assays: impact on myocardial infarction incidence and prognosis. Am J Med. 2012;125(12):1205-1213.e1. doi:10.1016/j.amjmed.2012.07.015 CrossRef Pubmed
40. Chew DP, Zeitz C, Worthley M, et al. Randomized Comparison of High-Sensitivity Troponin Reporting in Undifferentiated Chest Pain Assessment. Circ Cardiovasc Qual Outcomes. 2016;9(5):542-553. doi:10.1161/CIRCOUTCOMES.115.002488 CrossRef Pubmed
41. Bandstein N, Wikman A, Ljung R, Holzmann MJ. Survival and resource utilization in patients with chest pain evaluated with cardiac troponin T compared with high-sensitivity cardiac troponin T. Int J Cardiol. 2017;245:43-48. doi:10.1016/j.ijcard.2017.05.111 CrossRef Pubmed
42. Eggers KM, Lindahl B, Melki D, Jernberg T. Consequences of implementing a cardiac troponin assay with improved sensitivity at Swedish coronary care units: an analysis from the SWEDEHEART registry. Eur Heart J. 2016;37(30):2417-2424. doi:10.1093/eurheartj/ehw029 CrossRef Pubmed
43. Morrow DA, Bonaca MP. Real-world application of “delta” troponin. Diagnostic and prognostic implications. J Am Coll Cardiol 2013;62:1239–41. CrossRef Pubmed
44. Bradshaw PJ, Ko DT, Newman AM, Donovan LR, Tu JV. Validity of the GRACE (Global Registry of Acute Coronary Events) acute coronary syndrome prediction model for six month post-discharge death in an independent data set. Heart. 2006;92(7):905-909. doi:10.1136/hrt.2005.073122 CrossRef Pubmed
45. Antman EM, Cohen M, Bernink PJ, et al. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA. 2000;284(7):835-842. doi:10.1001/jama.284.7.835 CrossRef Pubmed
46. Writing Committee Members, Lawton JS, Tamis-Holland JE, et al. 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines [published correction appears in J Am Coll Cardiol. 2022 Apr 19;79(15):1547]. J Am Coll Cardiol. 2022;79(2):e21-e129. doi:10.1016/j.jacc.2021.09.006 CrossRef
47. Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization [published correction appears in Eur Heart J. 2019 Oct 1;40(37):3096]. Eur Heart J. 2019;40(2):87-165. doi:10.1093/eurheartj/ehy394 CrossRef Pubmed
48. Doll JA, Hira RS, Kearney KE, et al. Management of Percutaneous Coronary Intervention Complications: Algorithms From the 2018 and 2019 Seattle Percutaneous Coronary Intervention Complications Conference. Circ Cardiovasc Interv. 2020;13(6):e008962. doi:10.1161/CIRCINTERVENTIONS.120.008962 CrossRef Pubmed
49. Fox KA, Poole-Wilson P, Clayton TC, et al. 5-year outcome of an interventional strategy in non-ST-elevation acute coronary syndrome: the British Heart Foundation RITA 3 randomised trial. Lancet. 2005;366(9489):914-920. doi:10.1016/S0140-6736(05)67222-4 CrossRef Pubmed
50. Fox KA, Clayton TC, Damman P, et al. Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome a meta-analysis of individual patient data. J Am Coll Cardiol. 2010;55(22):2435-2445. doi:10.1016/j.jacc.2010.03.007 CrossRef Pubmed
SUPPLEMENTAL MATERIALS
Copyright Information
