Original Article
December 2020, 29:1
First online: 17 March 2021
Original Article
Preexisting Chronic Kidney Disease and Dyslipidemia are Strong Predictors for Early Acute Cerebrovascular Event After Isolated Coronary Artery Bypass Grafting: A Single Cardiac Center Experience
Leonardo Paskah Suciadi,a Andreas Hartanto Santoso,b Irvan Cahyadi,b Hoo Felicia Davina Hadi Gunawan,b Joshua Henrina Sundjaja,b Andreas Willianto,b Sylvie Sakasasmita,b Alex Komalasari,b Maizul Anwar,c Antono Sutandara
a Cardiology and Vascular Medicine Department of Siloam Hospital Kebon Jeruk, Jakarta, Indonesia
b Research Division of Siloam Heart Institute, Jakarta, Indonesia
c Cardiothoracic and Vascular Surgery Department of Siloam Hospital Kebon Jeruk, Jakarta, Indonesia
Correspondence: Leonardo Paskah Suciadi, Cardiologist, Siloam Heart Institute – Siloam Hospital Kebon Jeruk, Jl. Perjuangan No.8, RT.14/RW.10, Kb. Jeruk, Kec. Kb. Jeruk, Kota Jakarta Barat, Daerah Khusus Ibukota Jakarta 11530
Phone: +62821126590192 Fax: +6221-5300876
Email: be.bakerstreet@gmail.com
ABSTRACT
The outcomes of coronary artery bypass grafting (CABG) surgery are determined by numerous factors. This study aimed to analyze the factors contributing to short-term outcomes of patients undergoing isolated CABG. This retrospective analysis enrolled all adult patients undergoing isolated CABG at our center between January 2013 and December 2016. Clinical characteristics and postoperative events were recorded and analyzed. Overall, 242 patients (mean age, 59.7 ± 9.5 years) were included. The majority of the patients (88.4%) were men. The median left ventricular ejection fraction (LVEF) was 50% ± 15%, with 38% patients having an LVEF lower than 40% and 9.1% having an LVEF lower than 25%. The mean preoperative creatinine level was 1.25 ± 0.73, and the estimated glomerular filtration rate was 68.55 ± 23 ml/min/1.73 m2. The intensive cardiac care unit stay and total in-hospital stay were 70 ± 59 h and 8 ± 4 days, respectively. The in-hospital mortality rate was 2.1%. The most common major adverse events were new-onset atrial fibrillation (31.8%) and significant worsening of renal function (21.5%). Stroke occurred in 3.7% patients, for which preexisting chronic kidney disease (CKD) and dyslipidemia were strong predictors (P < 0.05; area under the curve [AUC], 87.7%). Advanced age and hypertension were considered significant risk factors for developing new-onset atrial fibrillation (P < 0.05; AUC 65%). Worsening renal function and new-onset atrial fibrillation were the most frequent complications that occurred during hospitalization following CABG. Preexisting CKD and dyslipidemia were the major risk factors for developing acute stroke post surgery. KEYWORDSAcute cerebrovascular events, Chronic kidney disease, Coronary artery bypass grafting, Dyslipidemia.
INTRODUCTION
Coronary artery disease (CAD) is one of the most common causes of death worldwide, including in Indonesia.1, 2 According to the National Basic Health Research in 2013, the diagnosis of CAD covered approximately 0.5% to 1.5% of cases in our country.3 The prevalence of this degenerative disease tends to increase along with older age, with the highest prevalence observed in the population aged 65 to 74 years old (3.6%).4 Patients with CAD have significantly higher rates of morbidity and mortality than the normal population across all ages. Management of patients with CAD includes medication and invasive procedures, including percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG).5 Clinical consideration and comprehensive discussion between cardiologists and cardiac surgeons are required to determine the best approach to manage patients with complex CAD. CABG was performed for the first time in 1960, with the purpose of alleviating symptoms, increasing quality of life, and improving the prognosis for CAD patients better than a conservative approach using medication.6–9 Currently, CABG is a routine surgical procedure for managing patients with complex CAD worldwide, including in Indonesia. Our cardiac center, Siloam Heart Institute of Siloam Hospitals Kebon Jeruk, has performed this procedure routinely since 2013. In our institution, there has been a significant increase in the number of CABG cases over time. Notably, our center has become one of the top referral hospitals for CABG in the West Region of Indonesia, especially in the Greater Jakarta area. In the general population, the in-hospital mortality rate for CABG is relatively low, but the mortality rate increases sharply if complications occur.10, 11 The most serious complications are related to the clinical profiles of patients, preexisting conditions, technical aspects of the surgery, and perioperative management in the critical care unit and inpatient ward.12–15 It is generally believed that the outcomes following CABG are affected by multifactorial issues. This study aimed to describe the clinical characteristics and analyze the essential factors contributing to short-term outcomes of patients undergoing isolated CABG. This report will be of value to add databases of clinical outcomes following CABG, especially in an Indonesian population. Thus, the results might lead to the development of a protocol to improve both the safety and efficacy of CABG.
METHODS
This retrospective cross-sectional study included all patients aged 18 years or older who underwent isolated CABG in our cardiac center, including on-pump and off-pump procedures, between January 2013 and December 2016. Data regarding the patient characteristics and pre-, peri-, and postoperative comorbidities were obtained from the medical records. The preoperative variables included in this study were age, clinical risk factors (i.e., hypertension, chronic kidney disease (CKD), dyslipidemia, smoking status, and diabetes mellitus), history of previous cardiovascular disease (i.e., previous myocardial infarction, stroke, and heart failure), echocardiographic findings (including left ventricular ejection fraction [LVEF]), and previous medication. The perioperative variables recorded in this study included drug or procedure use in the operating theater (inotropic, vasopressor, and intraaortic balloon counterpulsation/intra-aortic balloon pump) and technical data, such as aortic cross-clamp and cardiopulmonary bypass (CPB) time.
Postoperative outcomes were in-hospital mortality, defined as all-cause death during an index CABG hospitalization; total length of stay (LOS), defined as the difference in dates between discharge and admission; and major adverse events, including stroke, sustained ventricular tachycardia/ventricular fibrillation, new-onset atrial fibrillation (AF), acute kidney injury (AKI), and shock. New-onset AF is defined as AF occurring during the hospital stay following CABG in patients without previously documented AF. AKI is defined as an increased serum creatinine level greater than 1.5-fold from its preoperative baseline, or urine output less than 0.5 cc/kg/h for at least 6 consecutive hours.
Statistical analysis was conducted using the chi-squared test and multivariate logistic regression analysis. The chi-squared test was conducted to determine the independent variables according to major adverse events that were included in the logistic regression model. The independent variables in the logistic regression model were the variables with chi-square P-value less than 0.25. The final multivariate logistic regression model was assessed for its calibration, using the Hosmer–Lemeshow test, and its discrimination using the receiver operating characteristic curve. The Hosmer–Lemeshow test with a P-value greater than 0.05 was considered a good calibration; an area under the curve (AUC) of 0.8 to 0.9 was considered a strong discrimination. All statistical analyses were conducted using the SPSS statistical package software (IBM SPSS Statistics, version 22, IBM Corp., Armonk, NY).
RESULTS
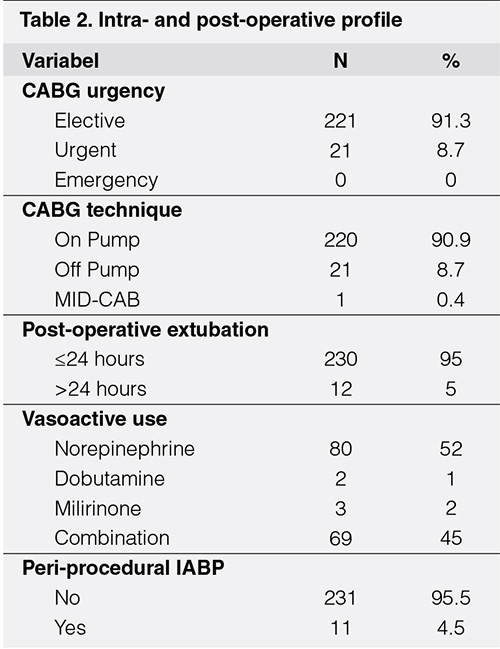
This study included a total of 242 patients undergoing isolated CABG during a 3-year study period at our cardiac center. The mean age of the patients was 59.7 ± 9.5 years, and the majority of the patients (88.4%) were men. The distribution of age and sex was similar between the groups with LVEF above and below 40% (Table 1). The youngest patient was 30 years old, whereas the oldest was 80 years old. Approximately 6% of the patients were classified as very elderly, as they were older than 75 years old. The mean body mass index of the patients was 24.86 ± 3.44 kg/m2; 28.1% of the patients were within the normal category, 24.0% were overweight, and 44.6% were classified as obese. Nearly half of our subjects were active smokers or had recently quit smoking.
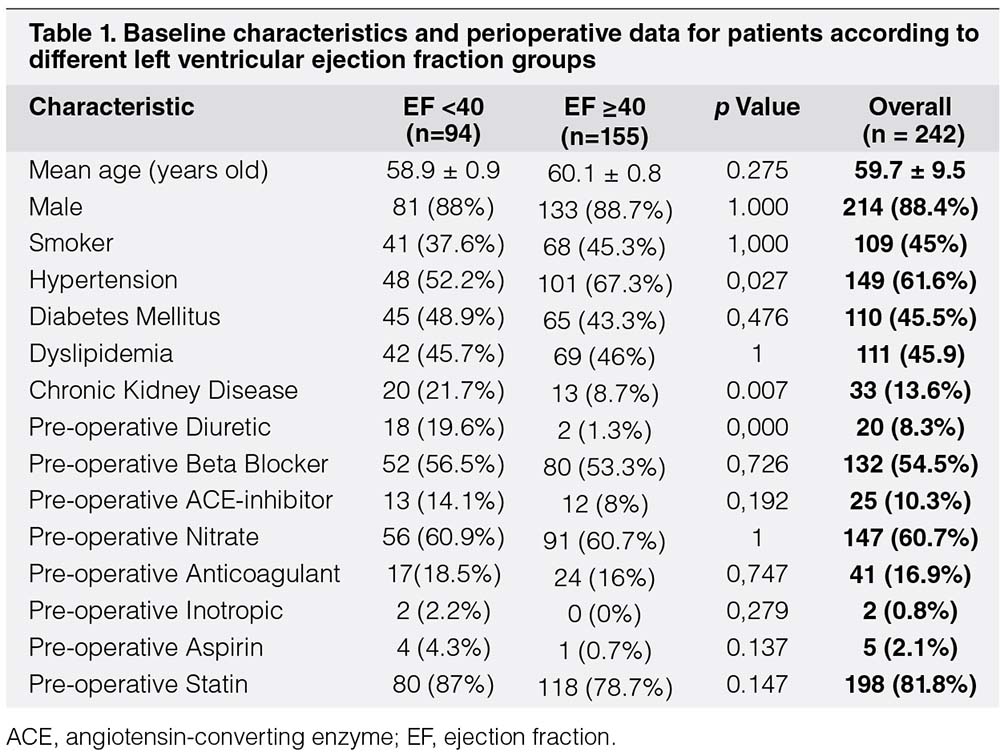
The median of LVEF measured using Simpson’s procedure from the apical four-chamber view of echocardiography was 50% ± 15%, with 38% of the patients having reduced ejection fraction lower than 40% and 9.1% of patients having poor left ventricular systolic dysfunction with LVEF lower than 25%. The mean preoperative creatinine level was 1.25 ± 0.73, and the estimated glomerular filtration rate was 68.55 ± 23 ml/min/1.73 m2. The common comorbidities observed among our patients were diabetes mellitus (45.5%), hypertension (61.6%), dyslipidemia (45.9%), previous myocardial infarction (45%), and previous stroke (9.6%) (Fig. 1). Hypertension was statistically more frequent in patients with LVEF of 40% or higher, whereas CKD with glomerular filtration rate below 60 ml/min/1.73 m2 was more common in the lower LVEF group (Table 1). In spite of the more frequent use of diuretics among patients with LVEF lower than 40%, no statistically significant difference was observed in the preoperative medication between the groups with lower and preserved LVEF.
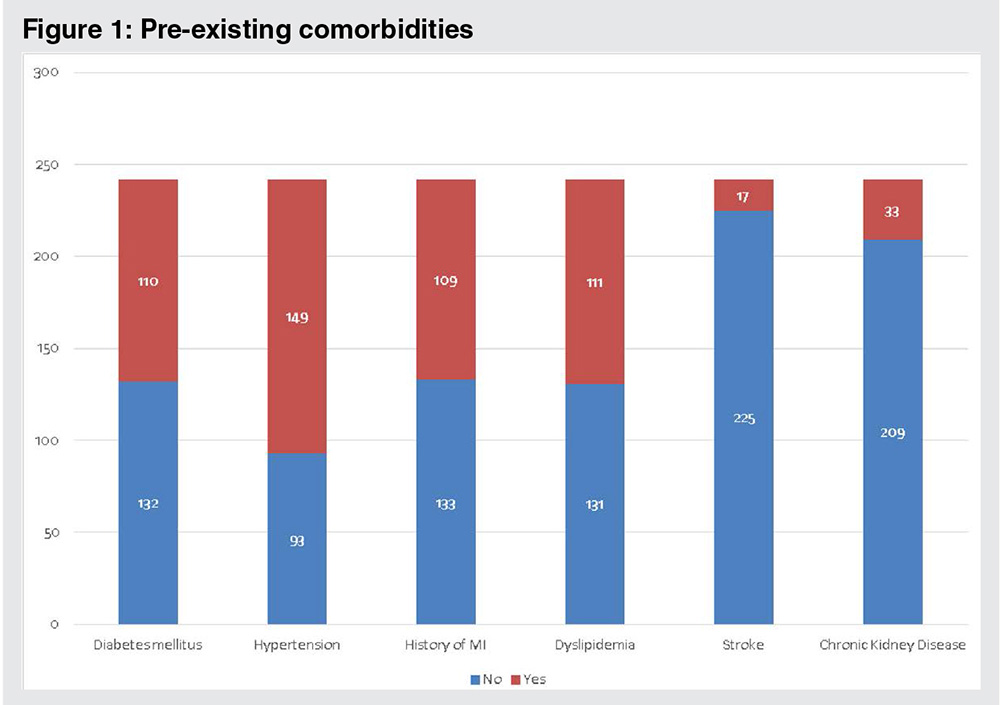
The majority of the patients (90.9%) underwent on-pump CABG, with only one case of minimally invasive approach CABG. Approximately 8.7% of the patients presented with recent acute coronary syndrome and were sent for urgent CABG. The median durations of CPB machine time and aortic cross clamping were 99 and 61 min, respectively (Table 2).
Postoperative requirement of vasoactive agents, including norepinephrine, dobutamine, dopamine, milrinone, or a combination, was noted in more than a half of the patients (63.2%) during the intermediate cardiac care unit (ICCU) stay. However, the use of vasoactive agents was temporary and only for the first few days following surgery in the majority of cases. The indications for using these agents were based on several reasons, including episodes of hypotension and an attempt to increase cardiac output with subsequently improved diuresis. Although intra-aortic balloon pump insertion was rarely used (4.5% cases), it was used preoperatively in four patients (36.36%), intraoperatively in five (45.45%), and postoperatively in two (18.18%). Almost all of the patients (95%) were successfully extubated within the first 24 h following surgery (Table 2). The length of ICCU stay and total in-hospital stay were 70 ± 59 h and 8 ± 4 days, respectively.
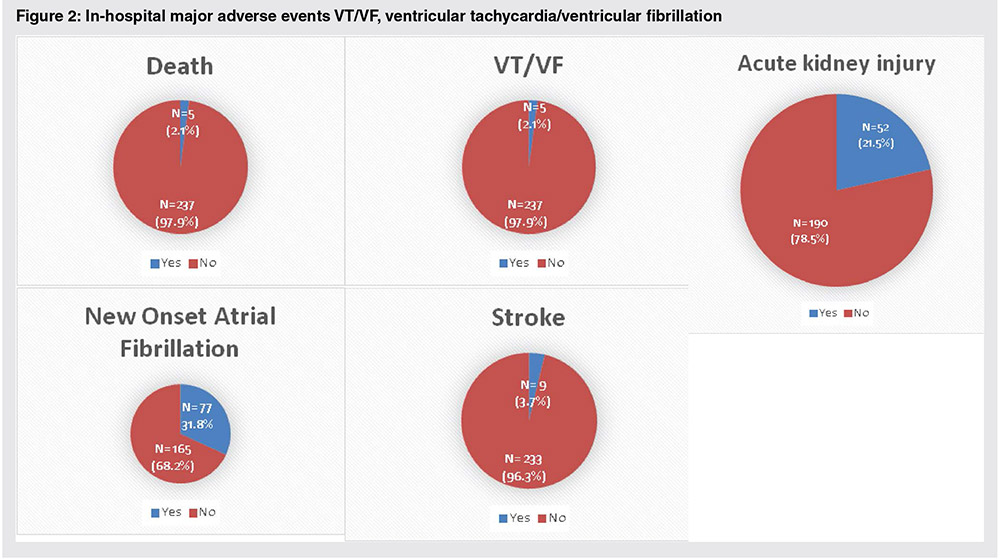
The in-hospital mortality rate following CABG was 2.1%. The most common major adverse events were new-onset AF (31.8%) and significantly worsening renal function (21.5%). In addition, debilitating non-hemorrhagic stroke occurred in 3.7% of the patients (Fig. 2). Data regarding persistent AF following discharge were lacking. No patients experienced worsening renal function requiring hemodialysis during the hospital stay.
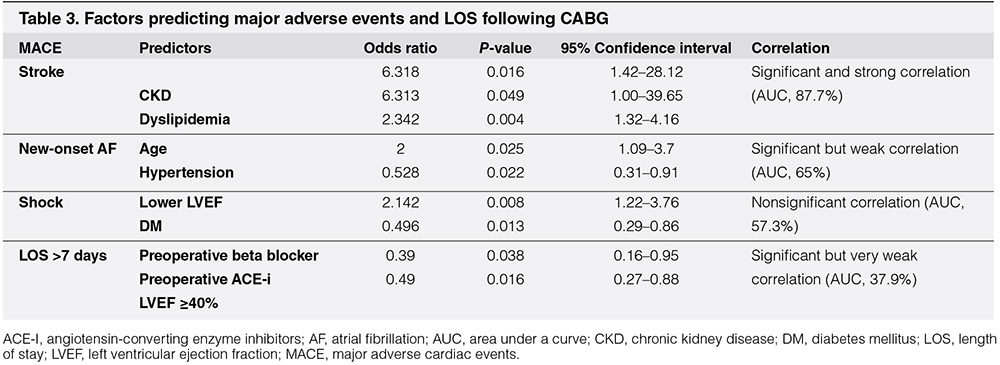
The variables in the logistic regression analysis were stroke, new-onset AF, cardiogenic shock, and prolonged hospital LOS. Multivariate analysis revealed several contributing factors which have a significant correlation with specific major adverse events following CABG. Preexisting CKD and dyslipidemia have a significant and strong correlation with the incidence of acute non-hemorrhagic stroke (P < 0.05; AUC, 87.7%). Increasing age and history of previous hypertension can also be considered predictors of higher new-onset AF events, although the correlation was weak (P < 0.05; AUC, 65%). Interestingly, there was a nonsignificant relationship between LVEF below 40% and shock following the procedure (P > 0.05; AUC, 57.3%). Meanwhile, preexisting diabetes mellitus significantly predicted hospital LOS greater than 7 days (odds ratio, 2.1), although this correlation was also weak. Contrarily, the use of preoperative beta-blocker and angiotensin-converting enzyme (ACE) inhibitor combined with a baseline LVEF of 40% or higher significantly, but weakly, correlated with shorter in-hospital LOS (P < 0.05; 37.9%) (Table 3).
DISCUSSION
The patients in this study were younger than populations in Western reports (mean age, 65 y),16 were predominantly male, were well nourished, and had modest LV systolic dysfunction and moderately impaired renal function. Almost all of our procedures were elective isolated CABG with the on-pump technique and median sternotomy approach. The in-hospital mortality rate reported at our center was 2.1%, which is comparable with the mortality rate following isolated CABG reported by the Society of Thoracic Surgeons (STS) Adult Cardiac Database 2017, which was 2.2% at centers with a similar level of volume cases.17 In addition, another report from several centers in Italy revealed that the 30-day mortality rate following CABG was approximately 2.61%.18 The in-hospital and 30-day mortality rates following CABG can be predicted using some validated risk models, such as EuroSCORE II (2012) calculation and the STS 2008 Cardiac Surgery Risk Model. The indicator variables used in these risk models include age, previous myocardial infarction, peripheral artery disease, renal insufficiency, heart failure, hemodynamic state, LVEF, complexity and urgency of the procedure, and some contributing comorbidities.19, 20
At our center, new-onset AF and worsening renal function were the most common complications following CABG. The incidence of new-onset AF in this study was within the range of 20% to 50% reported in the literature,21 but the incidence of AKI in this study (21.5%) was much higher than that in Western reports (2%–3%).21, 22 However, this complication was temporary, and hemodialysis was not indicated in all of the patients. Hemodialysis in the post-CABG period was as high as 27.2% in other reports.23 The significant number of patients experiencing AKI in this study can be explained by our use of looser criteria for worsening renal function according to the Acute Kidney Injury Network, which is generally used in medical–nonsurgical situations. AKI is defined as an increased creatinine level 1.5 times from baseline or urine output less than 0.5 cc/kg/h for at least 6 consecutive hours.24 Several reports using the Acute Kidney Injury Network criteria for defining worsening renal function following CABG showed varying incidence of AKI between 8% and 20%.25 However, the renal insufficiency that occurred in this population was temporary without progressive worsening and did not require hemodialysis until discharge. The mechanism of AKI following CABG is related to renal tubular injury caused by multifactorial conditions associated with preoperative profiles, intraoperative events, and early postoperative management, including the use of pharmacological agents.25-26 Preoperative factors included lack of renal reserve and preexisting renal insufficiency, which is commonly observed in patients with advanced age, diabetes mellitus, heart failure, and renovascular disease. Intraoperative factors related to the use of CPB include duration and specific details of perfusion technique and other complications during surgery, such as bleeding, hemodilution, and prolonged hypotension. Postoperative conditions, including the use of nephrotoxin agents, volume depletion or overload, hemodynamic instability, and systemic inflammation, also contribute to the incidence of AKI.26
In general, the risk of stroke related to CABG is higher than that of PCI.27 The incidence of non-hemorrhagic stroke following CABG was 1.3% in the STS CABG Adult Cardiac Surgery Database (2012).16 This number tends to decrease over time, and it was reported to be as low as 0.8% in the Veterans Affairs Medical Centers.28 This complication can be caused by macroembolization, microembolization, and cerebral hypoperfusion during the procedure.29 Known risk factors include advanced age, female sex, previous stroke, severe chronic pulmonary disease, diabetes mellitus, hypertension, and emergency surgery.21, 30 The strongest predictors for stroke events in this study were preexisting CKD and dyslipidemia, each of which could increase the risk of stroke by more than six times compared with those without these factors. The majority of stroke cases in this study had minor disability and temporary symptoms, and there were no cases with significant reduced level of consciousness at discharge.
AF is known to be the most common disturbing arrhythmia to occur following cardiac surgery. The incidence of new-onset AF following CABG ranges from 18% to 50%, depending on the means of examination.31, 32 AF usually occurs within the first 5 days following surgery, with a peak incidence on the second postoperative day.21 The predisposition factors of new-onset AF following CABG include elderly age, male sex, peripheral artery disease, chronic lung disease, concomitant valvular heart disease (especially mitral valves), significant left atrial enlargement, and previous cardiac surgery.33 In this study, patients with advanced age or history of hypertension had at least twice the risk for developing new-onset AF, although this correlation was statistically weak. Advanced age is associated with degenerative changes, such as fibrosis and dilatation, which affect the atrial electrophysiological characteristics.34 Meanwhile, long-standing hypertension is correlated with left ventricular hypertrophy, increased left ventricular filling pressure, and left atrial remodeling.35 Contrarily, the preoperative administration of some medications, including beta-blockers, ACE inhibitors, and statins, did not exhibit significant correlation with, or prevent, AF in this study.
One of the major drivers of hospital resource consumption following CABG care is hospital LOS. To improve healthcare efficiency, numerous institutions have implemented early discharge protocol. Therefore, LOS can indicate the quality of care of the center.21 Total in-hospital LOS at our center was still inefficient (average, 8 d), although the ICCU was considerably shorter (<3 d). In the Veterans Affairs Medical Centers, the in-hospital LOS was reported as a mean of 8 to 9 days, and the ICCU LOS was reported as a mean of 2 to 3 days.28 This resulted in an analysis of the factors contributing to prolonged LOS following CABG. Successful early extubation within the first 24 h in the majority of our patients may contribute to short ICCU LOS. We also found that diabetes mellitus indicated a significant correlation with the total LOS of more than 7 days. Patients with diabetes mellitus undergoing CABG had a two times higher incidence of prolonged LOS. Contrarily, preoperative beta-blocker and ACE inhibitor agents correlated with shorter in-hospital LOS following the procedure, although this correlation was statistically weak. Furthermore, patients with LVEF greater than 40% also revealed the benefit of shorter hospitalization. Conversely, as stated in some literature, patients with lower LVEF undergoing cardiac surgery are at a higher risk for postoperative complications and mortality following cardiac surgery.21, 35 However, in this study, we found that only lower ejection fraction exhibited a nonsignificant correlation with the incidence of shock after the surgery.
This study has several limitations. First, this evaluation came from a single-center experience and thus might not represent the characteristics and outcomes of CABG in the general population in Jakarta, or even in Indonesia. Second, the data were obtained by retrospectively reviewing conventional medical records. This impractical process limited the obtainment of some additional data or confirmation of previous findings. However, our center applied the standard of care in managing patients following cardiac surgery so that important data and evaluation were almost complete and standardized. Third, our experience was still limited in performing off-pump CABG and minimally invasive direct CABG. These methods were only indicated in the need of single CABG (commonly to the left anterior descending artery) in patients considered to have a high risk of stroke or renal insufficiency. Finally, follow-up after discharge was not available in this registry. Therefore, we do not know for certain the longer-term outcomes of these patients. Some patients still seek follow-up and medical care at our center regularly, and we can follow their conditions. However, the majority of patients came from different cities or even other islands. These patients usually visit other centers in remote areas after we referred them back.
CONCLUSION
This study analyzed the short-term clinical outcomes following isolated CABG in patients who were considerably younger than those in Western reports, who were predominantly men, who were well nourished, and who had modest left ventricular systolic dysfunction and moderately impaired renal function. The in-hospital mortality rate was comparable to other global reports. Nevertheless, the most common complications encountered were temporary worsening of renal function and new-onset AF. The incidence of AKI was remarkably higher than that which is widely reported, although none of our cases required hemodialysis. Preexisting CKD and dyslipidemia were identified as the major risk factors for developing acute non-hemorrhagic stroke following surgery.
REFERENCES
1. Finegold JA, Asaria P, Francis DP. Mortality from ischaemic heart disease by country, region, and age: statistics from World Health Organisation and United Nations. Int J Cardiol 2013;168:934-945. CrossRef Pubmed
2. Roth GA, Huffman MD, Moran AE, Feigin V, Mensah GA, Naghavi M, Murray CJL. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation 2015;132:1667-1678. CrossRef Pubmed
3. Ministry of Health Republic of Indonesia. Indonesia Health Profile 2013 [Internet]. [cited 2018 Nov 4]. Available from: http://www.depkes.go.id/resources/download/pusdatin/profil-kesehatan-indonesia/Indonesia%20Health%20Profile%202013%20-%20v2%20untuk%20web.pdf
4. Ministry of Health Republic of Indonesia. Hasil Riskesdas 2013. [Internet]. [cited 2018 Nov 4]. Available from: http://www.depkes.go.id/resources/download/general/Hasil%20Riskesdas%202013.pdf
5. Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Ju ni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 2019;40:87-165. CrossRef Pubmed
6. Squiers JJ, Mack MJ. Coronary artery bypass grafting—fifty years of quality initiatives since Favaloro. Ann Cardiothorac Surg 2018;7:516-520. CrossRef Pubmed
7. Aksut B, Starling R, Kapadia S. Stable coronary artery disease and left ventricular dysfunction: The role of revascularization. Catheter Cardiovasc Interv 2017;90:777-783. CrossRef Pubmed
8. Baig K, Harling L, Papanikitas J, Attaran S, Ashrafian H, Casula R, Athanasiou T. Does coronary artery bypass grafting improve quality of life in elderly patients? Interact Cardiovasc Thorac Surg 2013;17:542-553. CrossRef Pubmed
9. Petrie MC, Jhund PS, She L, Adlbrecht C, Doenst T, Panza JA, Hill JA, Lee KL, Rouleau JL, Prior DL, Ali IS, Maddury J, Golba KS, White HD, Carson P, Chrzanowski L, Romanov A, Miller AB, Velazquez EJ. Ten year outcomes after coronary artery bypass grafting according to age in patients with heart failure and left ventricular systolic dysfunction: an analysis of the extended follow up of the STICH trial. Circulation 2016;134:1314-1324. CrossRef Pubmed
10. Dos Santos CA, de Oliveira MAB, Brandi AC, Botelho PHH, Brandi J de CM, dos Santos MA, Godoy MF, Braile DM. Risk factors for mortality of patients undergoing coronary artery bypass graft surgery. Rev Bras Cir Cardiovasc Órgão Of Soc Bras Cir Cardiovasc 2014;29:513-520. CrossRef Pubmed
11. Mazzeffi M, Zivot J, Buchman T, Halkos M. In-hospital mortality after cardiac surgery: patient characteristics, timing, and association with postoperative length of intensive care unit and hospital stay. Ann Thorac Surg 2014;97:1220-1225. CrossRef Pubmed
12. Tsai I-T, Wang C-P, Lu Y-C, Hung W-C, Wu C-C, Lu L-F, Chung F-M, Hsu C-C, Lee Y-J, Yu T-H. The burden of major adverse cardiac events in patients with coronary artery disease. BMC Cardiovasc Disord [Internet]. 2017 [cited 2018 Nov 4];17. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5210314/
CrossRef
Pubmed
13. Shroyer AL, Hattler B, Wagner TH, Collins JF, Baltz JH, Quin JA, Almassi H, Kozora E, Bakaeen F, Cleveland Jr JC, Bishawi M, Grover FL. Five-year outcomes after on-pump and off-pump coronary-artery bypass. N Engl J Med 2017;377:623-632. CrossRef Pubmed
14. Gurbuz O, Kumtepe G, Ercan A, Yolgosteren A, Ozkan H, Karal IH, Ercan A, Ener S. A comparison of off- and on-pump beating-heart coronary artery bypass surgery on long-term cardiovascular events. Cardiovasc J Afr 2017;28:30-35. CrossRef Pubmed
15. Smilowitz Nathaniel R, Berger Jeffrey S. Perioperative management to reduce cardiovascular events. Circulation 2016;133:1125-1130. CrossRef Pubmed
16. ElBardissi AW, Aranki SF, Sheng S, O’Brien SM, Greenberg CC, Gammie JS. Trends in isolated coronary artery bypass grafting: an analysis of the society of thoracic surgeons adult cardiac surgery database. J Thorac Cardiovasc Surg 2012;143:273-281. CrossRef Pubmed
17. Shahian DM, O’Brien SM, Normand SL, Peterson ED, Edwards FH. Association of hospital coronary artery bypass volume with processes of care, mortality, morbidity, and the Society of Thoracic Surgeons composite quality score. J Thorac Cardiovasc Surg 2010;139:273-282. CrossRef Pubmed
18. Seccareccia F, Perucci CA, D’Errigo P, Arcà M, Fusco D, Rosato S, Greco D. The Italian CABG Outcome Study: short-term outcomes in patients with coronary artery bypass graft surgery. Eur J Cardiothorac Surg 2006;29:56-62. CrossRef Pubmed
19. Nashef SAM, Roques F, Sharples LD, Nillson J, Smith C, Goldstone AR, Lockowandt U. EuroSCORE II. Eur J Cardiothorac Surg 2012;41:734-745. CrossRef Pubmed
20. Shahian DM, O’Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand S-L T, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP, for the Society of Thoracic Surgeons Quality Measurement Task Force. The Society of Thoracic Surgeons 2008 cardiac surgery risk models. Ann Thorac Surg 2009;88:2-22. CrossRef Pubmed
21. Hillis LD, Smith PK, Anderson JL, Bitti JA, Bridges CR, Byrne JG, Cigarroa JE, DiSesa VJ, Hiratzka LF, Hutter Jr. AM, Jessen ME, Keeley EC, Lahey SJ, Lange RA, London MJ, Mack MJ, Patel MR, Puskas JD, Sabik JF, Selnes O, Shahian DM, Trost JC, Winniford MD. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery: Executive Summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011;124:2610-2642. CrossRef Pubmed
22. Abraham VS, Swain JA. Cardiopulmonary bypass and kidney. In: Gravlee GP, Davis R, eds. Cardiopulmonary Bypass: Principles and Practice. Philadelphia, PA: Lippincott, Williams & Wilkins, 2000:382-391.
23. Jose R, Shetty A, Khrisna N, Chathoth V, Bhaskaran R, Jayant A, Varma PK. Early and mid‐term outcomes of patients undergoing coronary artery bypass grafting in ischemic cardiomyopathy. J Am Heart Assoc 2019:8:e010225. CrossRef Pubmed
24. Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A. Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Critical Care 2007;11. CrossRef Pubmed
25. Mao H, Katz N, Ariyanon W, Blanca-Martos L, Adýbelli Z, Giuliani A, Danesi TH, Kim JC, Nayak A, Neri M, Virzi GM, Brocca A, Scalzotto E, Salvador L, Ronco C. Cardiac surgery-associated acute kidney injury. Cardiorenal Med 2013;3:178-199. CrossRef Pubmed
26. Rosner MH, Okusa MD. Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol 2006;1:19-32. CrossRef
27. Naghshtabrizi B, Sohrabi Z, Emami F, Manafi B, Membari S, Naghshtabrizi B. Evaluation of the incidence of major adverse cardiac and cerebrovascular events after percutaneous coronary intervention or coronary artery bypass graft on proximal left anterior descending artery with and without others coronary arteries involvement. Int Cardiovasc Res J 2016:10:e10281.
28. Lushaj EB, Schreiner A, Jonuzi B, Badami A, DeOliveira N, Lozonschi L. Short-term clinical outcomes after off-pump coronary artery bypass grafting at a single Veterans Affairs Medical Center. J Cardiothorac Surg 2016;11:1-4. CrossRef Pubmed
29. Gottesman RF, Sherman PM, Grega MA, Yousem DM, Borowicz Jr. LM, Selnes OA, Baumgartner WA, McKhann GM. Watershed strokes after cardiac surgery: diagnosis, etiology, and outcome. Stroke 2006;37:2306-2311. CrossRef Pubmed
30. Filsoufi F, Rahmanian PB, Castillo JG, Bronster D, Adams DH. Incidence, topography, predictors and long-term survival after stroke in patients undergoing coronary artery bypass grafting. Ann Thorac Surg 2008;85:862-870. CrossRef Pubmed
31. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener H-C, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Putte BV, Vardas P. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016;37:2893-2962. CrossRef Pubmed
32. Kosmidou I, Chen S, Kappetein AP, Serruys PW, Gersh BJ, Puskas JD, Kandzari DE, Taggart DP, Morice M-C, Buszman PE, Bochenek A, Schampaert E, Page P, Sabik JF, McAndrew T, Redfors B, Ben-Yehuda O, Stone GW. New-Onset Atrial Fibrillation After PCI or CABG for Left Main Disease: The EXCEL Trial. J Am Coll Cardiol 2018;71:739-748. CrossRef Pubmed
33. Curtis AB, Rich MW. Atrial fibrillation in the elderly: Mechanisms and Management. Heart Rhythm 2007;4:1577-1579. CrossRef Pubmed
34. Ogunsua AA, Shaikh AY, Ahmed M, McManus DD. Atrial fibrillation and hypertension: mechanistic, epidemiologic, and treatment parallels. Methodist Debakey Cardiovasc J 2015;11:228-234. CrossRef Pubmed
35. Pieri M, Belletti A, Monaco F, Pisano A, Musu M, Dalessandro V, Monti G, Finco G, Zangrillo A, Landoni G. Outcome of cardiac surgery in patients with low preoperative ejection fraction. BMC Anesthesiol 2016;16:97. CrossRef Pubmed
Figure LegendsFigure 1. Preexisting comorbidities
Figure 2. In-hospital major adverse events VT/VF, ventricular tachycardia/ventricular fibrillation.
Copyright Information
