Original Article
December 2020, 29:1
First online: 17 March 2021
Original Article
Clinical Profile and Cost of Treatment among Patients with Lymphedema in Philippine Heart Center from 2018-2020
Bryan Rene F. Toledano M.D (Senior Adult Cardiology Fellow in training),1 Catherine V. Sta Monica R.N CLT (Registered Nurse, Certified Lymphatic Therapist),1 Gertie May B. Plameras M.D (Consultant - Adult Cardiology, Vascular)1
1 Philippine Heart Center
Email address: imbryantoledano@gmail.com, phcresearch@gmail.com
Contact number: 09054776260
ABSTRACT
PURPOSEThis is a local study conducted that describes the clinical profile and cost incurred of patients with lymphedema among Filipinos seen in our institution.
METHODSA descriptive study using the data from the Philippine Heart Center Lymphedema clinic from 2018-2020. It consists of the patient’s name, age, sex, lymphedema onset, classification, type, stage, affected site, treatment modality, and the number of sessions. The cost incurred was based on the clinic’s costing list, treatment modality, and the number of sessions rendered.
RESULTSThe analysis included a total of 97 patients. The mean age was 60.3 (± 14.3) years old, with female predominance (74.2% versus 25.8%). The majority is classified as secondary (91.8%) versus primary (8.2%). The classification of primary lymphedema are praecox (62.5%), congenital (25%) and tarda (12.5%) while for secondary it is cancer related (53.9%), phlebolymphedema (34.8%), lipolymphedema (3.4%), obesity induced 3.4%, trauma related, infection (3.4%) and iatrogenic (1.1). The stage of severity is stage IIA (60.8%), III (17.6%), IIB (13.4%), and I (8.2%). The most affected site is bilateral lower extremities (30%), followed by left (18.5%) and right (17.5%) lower extremities. The right and left upper extremities showed equal (16.5%) with no bilateral upper extremities affectation. The majority of treatment is unilateral (68.8%) versus bilateral (31.2%) decompressive lymphatic therapy. The total cost incurred was an average of P17,753 per patient and mostly came from the private section (89.7%) versus (10.3%).
CONCLUSIONLymphedema is a chronic and recurrent disease that carries a substantial cost to patients. Its exact incidence, treatment outcomes, and quality of life among Filipinos are yet to be explored. A clinical profile will be the first step to raise awareness and to identify the different subset of populations for prevention, support, and treatment.
KeywordsClinical profile, Cost of treatment, Lymphedema
INTRODUCTION
Lymphedema is an abnormal homeostasis of the lymphatic circulation that causes a collection of clinical and pathologic manifestations. The elucidation of the lymphatic system’s distinct anatomical and physiologic complexity provides the pathogenesis of its edema and features that differentiate it from other diseases.1 The cascade starts when lymphatic fluids accumulate in the interstitial space, causing inflammation, adipose tissue deposition, and fibrosis to the surrounding tissues.2 It is a chronic, progressive, and debilitating disease that may have a large impact on one’s physical, emotional, social, psychological, and financial aspects.3 It was only recently that this orphan disease was adopted by vascular medicine together with plastic surgery, rehabilitation medicine, and dermatology specialty. However, it is still often overlooked due to lack of knowledge and the clinical impact underestimated.4 The available pieces of literature are scant and only a handful was published. These studies explored lymphedema in terms of its incidence, prevalence, epidemiology, and the associated quality of life.5, 6, 7, 8, 9, 10 In the Philippines, few centers cater to patients with this kind of disease. One of which is the Philippine Heart Center. In late 2017 a new service of the division of vascular medicine, the Lymphedema Clinic was established. It offers consultation from a vascular medicine adult cardiology lymphedema specialists and complex lymphatic therapy performed by our lymphedema therapist consisting of manual lymphatic drainage, compression therapy, skincare, and exercise and self-management.11 The clinical profile and cost of treatment would be useful to raise awareness and plan potential interventions in the coming future.
METHODOLOGY
The census from the lymphedema clinic of the Philippine Heart Center from January 2018 to March 2020 will be used. It consists of the name, age, sex, onset, lymphedema classification, stage, affected site, treatment modality, and the number of sessions. For data extraction, a data collection form will be used. Each patient will be assigned a code. The computation of the direct cost is based on the number of affected limbs, the number of sessions completed, type of treatment modality prescribed regardless if its upper or lower extremities (eg. unilateral vs bilateral), and the cost of the treatment modality as listed in our outpatient costing list (e.g. unilateral decompressive lymphatic drainage P2,200, bilateral decompressive lymphatic drainage P3,500) from January 2018-March 2020. Definition of terms- Lymphedema – a chronic disease marked by increased collection of lymphatic fluid in the body, causing swelling which can lead to skin and tissue changes.10
- Primary lymphedema – an inherited or congenital condition that causes malformation of the lymphatic system, most often because of a gene mutation. It can be subdivided based on onset congenital if present at birth, praecox if during puberty or the beginning of 3rd decade and tarda which begins after 35 years of age 5.
- Secondary lymphedema – results from insult, injury or obstruction to the lymphatic system.1
- International Society of Lymphology (ISL) Stages11 – I : accumulation of tissue fluid with higher protein content, which subsides with limb elevation
- Decongestive lymphatic therapy (DLT) – is a program that combines the different treatment approach for lymphedema which includes manual lymphatic drainage, bandaging, compression pump, exercise and self-care10
- Phlebolymphedema- is a mixed-etiology swelling due to chronic venous insufficiency and lymphatic insufficiency. It is due to inability of lymphatic system to adequately drain the interstitial fluid that accumulates in severe chronic venous hypertension12
- Lipo-lymphoedema- a long term condition of abnormal build-up of fat cells that affects the lymphatic drainage13
- Obesity induced lymphedema- lymphedema caused by increased body mass index14
- Trauma related and iatrogenic lymphedema-accumulation of interstitial fluid secondary to disruption from trauma or iatrogenic injections3
- Infection induced lymphedema – accumulation of interstitial fluid secondary to inflammation of lymphatic channels from infection (bacteria, myocobacteria, virus, fungi and parasites3
- Cost incurred- number of sessions completed multiplied by the cost of treatment modality prescribed based on the affected number of limbs (eg unilateral or bilateral) regardless if its upper or lower extremities. (Unilateral DLT- P2,200; Bilateral DLT P3,500)
IIa : limb elevation alone rare reduces swelling and pitting is manifest
IIb : limb may or may not pit as fat and fibrosis supervenes
III : lymphostatic elephantiasis, the tissue is fibrotic, and pitting is absent. Skin thickening, hyperpigmentation, increased skin folds, fat deposits and warty overgrowth develop
The data obtained were listed and categorized using Microsoft Excel (version 16.38). The rechecking of data was done twice to ensure correctness and validity.
Statistical AnalysisAll analyses were performed using Microsoft Excel (version 16.38). A descriptive statistics was utilized to summarize data in quantitative form (e.g. age). while frequency and percentage summarized the data in categorical form.
RESULTS
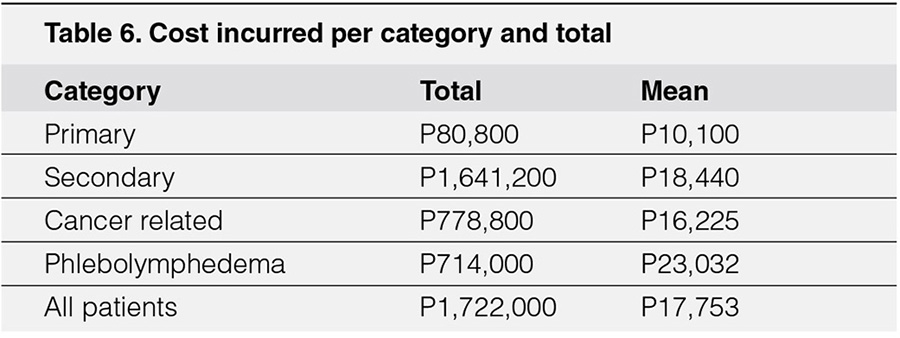
The analysis included a total of 97 individuals with the complete data needed. Their clinical profile is summarized. (Table-1). The mean age was 60.3 (± 14.3) years old, with female predominance (74.2% versus 25.8%) male. The majority is classified as a secondary cause of lymphedema (91.8%) versus primary (8.2%). The stage of severity in descending order are as follows stage IIA (60.8%), III (17.6%), IIB (13.4%), and I (8.2%). The most affected site is bilateral lower extremities (30%), followed by left (18.5%) and right (17.5%) lower extremities. The right and left upper extremities showed equal affectation (16.5%) while bilateral upper extremities showed none. Hence most treatment is unilateral (68.8%) versus bilateral (31.2%) decompressive lymphatic therapy. The total cost incurred is P1,722,000, an average of P17,753 per subject. The majority came from the private section (89.7%) versus service (10.3%).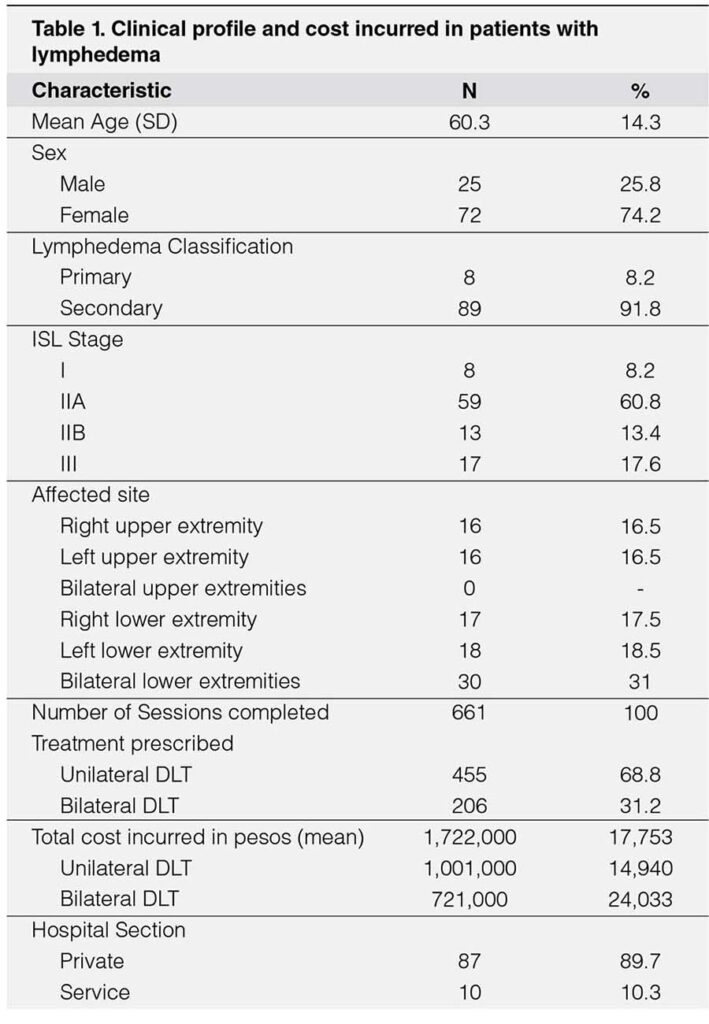
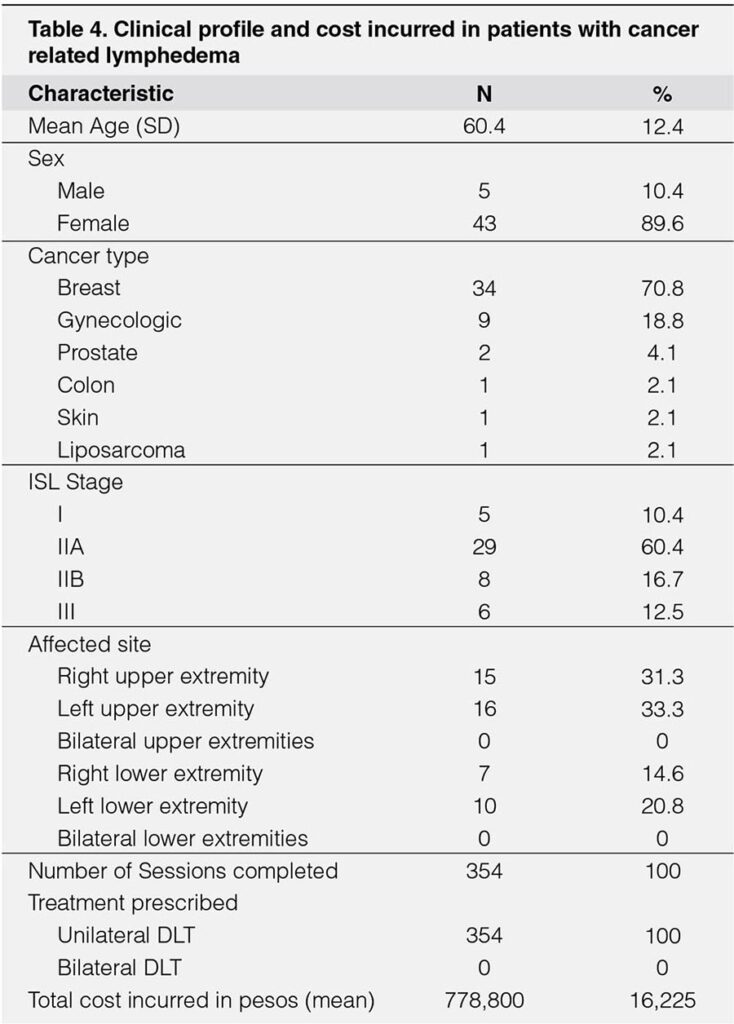
The analysis of subjects with cancer-related lymphedema included a total of 48 individuals. Their clinical profile is summarized. (Table-4). The mean age was 60.4 (± 12.4) years old, with female predominance (89.6%) versus (10.4%) male. The cancer type in descending order is as follows breast (70.8%), gynecologic (18.8%), prostate (4.1%), colon, prostate, and liposarcoma are equal (2.1%). For the severity of IIA (60.4%), IIB (16.7%), III (12.5%), and I (10.4%). The most affected site is left upper (33.3%), followed by right upper (19.1%), left lower (20.8%), right lower (14.6%) extremities. There are no bilateral upper and lower extremities documented. The estimated total cost incurred is P778,800 with an average of P16,225 per individual.
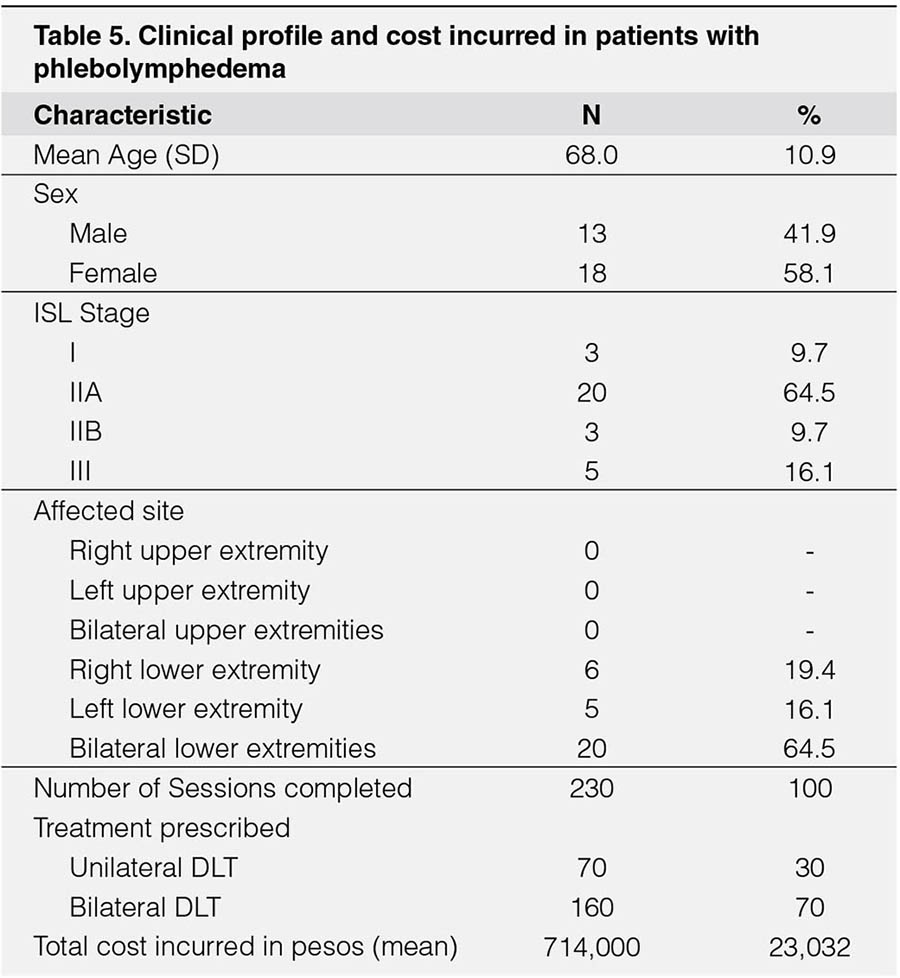
The analysis of subjects with phlebolymphedema included a total of 31 individuals. Their clinical profile is summarized. (Table-5). The mean age was 68.4 (± 10.9) years old, with slight female predominance (58.1%) versus (41.9%) male. The severity in descending order is as follows IIA (60.4%), III (16.1%), IIB, and I (9.7%). The most affected site is bilateral lower extremities (64.5%), followed by right (19.4%), left (16.1%) lower extremities. The estimated total cost incurred is P714,000 with an average of P23,032 per individual.
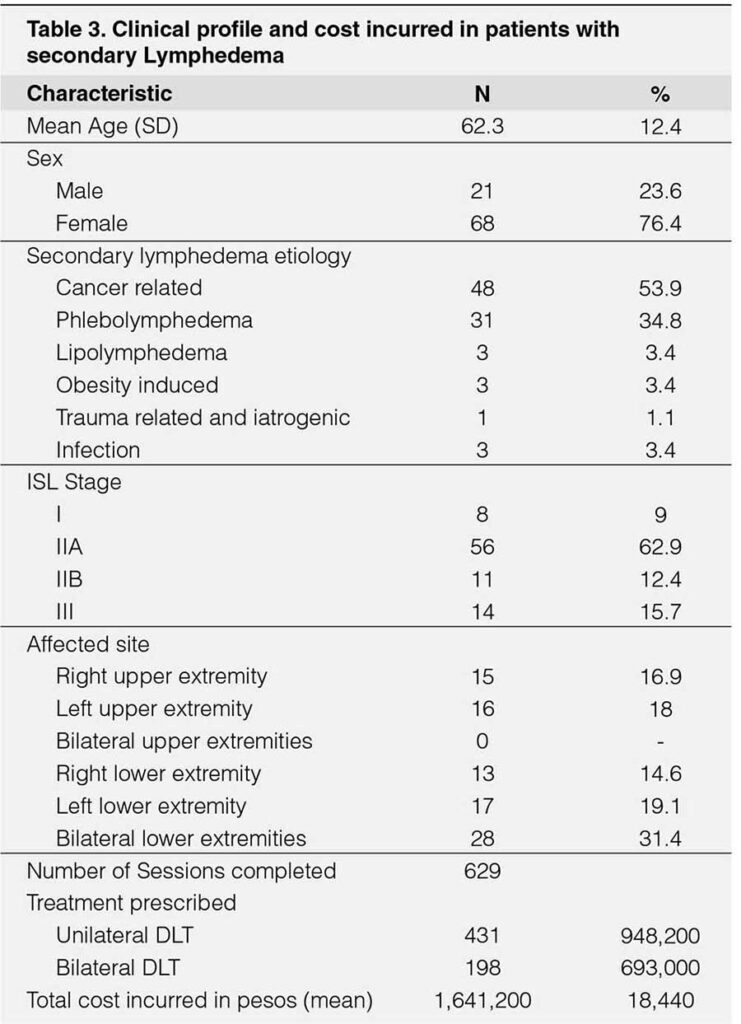
The estimated total cost in all patients is 1,722,000 pesos and a mean of 17,753 pesos per individual. It is highest among the secondary group 1,641,200 pesos followed by cancer-related 778,800 pesos, phlebolymphedema 714,00 pesos and lowest in primary group 80,800 pesos. The mean is highest in the phlebolymphedema 23,032 pesos followed by secondary 18,440 pesos, cancer-related 16,225 pesos, and lowest in primary group 10,100 pesos per individual.
DISCUSSION
The Philippine Heart Center is a specialized hospital that caters to cardiovascular patients, one of its department is vascular medicine within it is the lymphedema clinic. Our vascular adult cardiologists serve as the lymphedema specialist. The diagnosis is primarily made based on history and physical examination. Typical clinical features such as persistent edema of more than three months, minimal response to elevation or medications, presence of skin changes, and asymmetric limb measurements are sought. 3 Additional imaging of lymphoscintigraphy is warranted to diagnose in the early stage of the disease or if it is unresponsive to treatment. A deep venous thrombosis screening using ultrasound is also done to exclude its presence.1 The average age of patients seen belongs to the elderly group (60.3) years old, with a female predominance. The positive association for age and increase incidence in women is probably due to the comorbidities or diseases that linked or have caused the lymphedema.5 Most patients are classified under secondary since it is composed of more common diseases compared to primary which are due to some rare genetic or syndromic entities.5 The stage of severity seen is mostly from moderate to severe (IIA-III) and only a few were mild (I). This is probably due to the symptoms, physical and psychological turmoil experienced by the patients that led to consultation and treatment.10 The most affected site is bilateral lower extremities which is the same with other studies,8 , 9 a higher gravitational pull may be contributory to lymphedema and further stasis.21 A unilateral affection of the left and right legs compared to arms shows only a slight difference. The affectation of the arms is less prevalent probably due to a greater number of lymph nodes, preferential usage, and its proximity to the thoracic duct for drainage. Also, no bilateral upper extremity affectation was documented. Our lymphatic therapist mostly performed unilaterally over bilateral decompressive lymphatic therapy depending on the localization. A DLT is the standard of care and further treatment is based on the outcome and recurrence of lymphedema. Monitoring of outcome can be measured using a circumferential tape measure and devices such as tonometry and bioimpedance.25 The cost incurred was based on the number of sessions and the type of treatment rendered. A unilateral DLT cost about P2,200 while a bilateral DLT a little higher P3,500. The cost does not include the transportation fee, nor the additional treatment cost of the primary disease or the complications of lymphedema such as recurrent skin infections.10 However certain discounts are made for senior and service patients. A total of P1,722,000 with an average of P17,753 per patient was incurred. The referral of patients mainly came from the private compared to the service section. The lack of awareness and exposure from the cardiology fellow in training and other physicians may be a contributing factor to this observation aside from the affordability of the treatment.
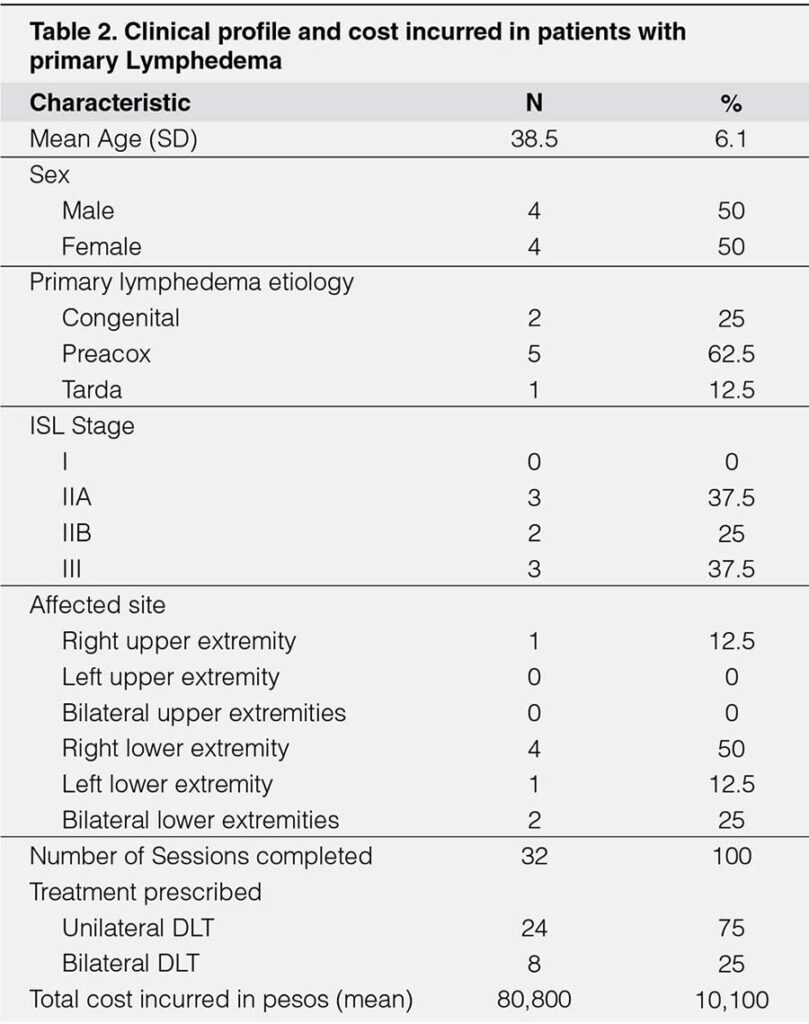
The patients with primary lymphedema included only a total of 8. It affects an estimated 1 in 100,000 people.5 The average age of patients seen belongs to the young adult 38.5 years old with no gender predilection.5 The diagnosis is suspected when the onset of edema occurs at a young age with no apparent cause. A culprit genetic mutation is usually not investigated, due to a lack of resources in our setting. A family history together with possible physical examination pointing to a syndrome provides valuable clues. The lymphoscintigraphy showing lymphatic hypoplasia with no or delayed lymph drainage confirms the diagnosis. Two patients were diagnosed with congenital lymphedema or Milroy’s disease. It is a rare autosomal dominant condition presenting with usually unilateral lower extremity lymphedema, up slanting toenails, papilloma, and prominent leg veins. 16 Five patients or 62.5% of primary lymphedema were diagnosed with praecox or Meigs disease. It is the most common form of primary lymphedema accounting for 65-80% of cases.5 It usually presents as unilateral leg swelling and females are more affected suggesting a hormonal effect on its pathogenesis.17 Among the five one is diagnosed with Klippel-Trenaunay syndrome. It is diagnosed clinically with the presence of port wine stains, unilateral leg hypertrophy of the bone, and soft tissue.18 Only one was diagnosed with lymphedema tarda presenting with painless, progressive swelling of the right leg during his 4th decade of life, similar to a case report.19 The cost of treatment incurred was an average of P10,100 the lowest among all groups. This observation may be due to the improvement of lymphatic drainage over time seen in some of the young patients as reported in a case report.20
The majority of patients seen have secondary lymphedema. The average age belongs to the elderly group with a female predominance. The gender predilection can be explained with the association of the etiology of secondary lymphedema. The most common is cancer-related secondary to breast and gynecologic malignancies. It occurs due to radical surgery, node dissection, and radiotherapy as observed with other cancer treatment complications of prostate, colon, skin, and liposarcoma.5 The most studied is breast cancer in which a cumulative incidence of 13.5% after two years, 30.2% after five years, and 41.1% after 10 years post-treatment are observed.21 The second most common is phlebolymphedema, an institutional bias that may be at play since chronic venous insufficiency (CVI) is a common disease treated by a vascular adult cardiologist. In CVI a loss of valvular function of the lower extremities may result from age-related, occult, or previous deep venous thrombosis (DVT) and surgery. The incidence is approximately 6% to 7% at 50 years of age, 20% at age 70 with a slight female preponderance possibly due to estrogen effect. It has the highest average cost incurred at P23,032 among all groups which are probably due to factors aggravating the condition such as heart failure, cirrhosis, or nephropathy.22
Although lymphatic filariasis is the most common cause of secondary lymphedema in the world5 only one out three infectious related was seen since it is not endemic in our region23 the remaining were due to bacterial lymphangitis. Minor etiologies with no known general incidence except for few observational studies are lipolymohedema it is an abnormal asymmetric fat distribution that leads to lymphedema if left untreated. It almost exclusively occurs in females during puberty or pregnancy.24 Obesity-induced due to lymphatic dysfunction is said to occur when the BMI threshold reaches between 53-59.16 Lastly, one iatrogenic cause occurred due to the injection of collagen in the buttocks and thighs for an aesthetic purpose which seldomly occurs. In terms of financial burden countries from the US and Europe assists thru statutory health insurances and takes into account direct and indirect costs.26, 27 In our institution, patients use their out-of-pocket money and grants obtained from the government.
CONCLUSION
Lymphedema is a chronic and recurrent disease that carries a substantial cost to patients. Its exact incidence, treatment outcomes, and quality of life among Filipinos are yet to be explored. A clinical profile will be the first step to raise awareness and to identify the different subset of populations for prevention, support, and treatment.
REFERENCES
1. Creager M, Beckman J, Loscalzo J. Vascular Medicine: A Companion to Braunwald’s Heart Disease 2nd 2012. Saunders.
2. Azhar SH, Lim HY, Tan BK, Angeli V. The unresolved pathophysiology of lymphedema. 2020. Frontiers in physiology. Vol 11. Article 137. CrossRef Pubmed
3. Moffat CJ, Franks PJ, Doherty DC, Williams AF, Badger C, Jeff’s E, et al. Lymphedema: an underestimated health problem. 2003. QJM 96: 731-738. CrossRef Pubmed
4. Földi E. Lymphatic Vascular Diseases. 2002. In: Lanzer P., Topol E.J. (eds) Pan Vascular Medicine. Springer, Berlin, Heidelber.
5. Rockson SG, Rivera KK. Estimating the Population Burden of Lymphedma. 2008. Ann N.Y. Acad Sci. CrossRef Pubmed
6. Pandey RA, Shrestha S. Prevalence of Arm Lymphedema among Patients with Breast Cancer Surgery. 2016. Journal of College of Medical Sciences-Nepal Vol12No3.
7. Quere I, Palmier S, Noerregaard S, Pastor J, Sykorova M, Mres MA, et al. LIMPRINT: Estimation of the Prevalence of Lymphedema/Chronic Edema in Acute Hospital in In-Patient. 2019. Lymphatic Research and Biology. V17No2. CrossRef Pubmed
8. Stolldorf DP, Dietrich MS, Ridner SH. Symptom Frequency, Intensity and Distress in Patients with Lower Limb Lymphedema. 2016. Lymphatic Research and Biology. Vol 14No2. CrossRef Pubmed
9. Stolldorf DP, Dietrich MS, Ridner SH. A comparison of the quality of life in patients with primary and secondary lower-limb lymphedema. A mixed-methos study. 2016. West J Nurs Res. CrossRef Pubmed
10. Mercier G, Pastor J, Moffat C, Franks P, Quere I. LIMPRINT: Health-Related Quality of Life in Adult Patients with Chronic Edema. 2019. Mary Ann Liebert, Inc. CrossRef Pubmed
11. Vascular Center. 2017. Retrieved from URL phc.gov.ph/services/vtour/vascular-center.php
12. Sleigh BC, Manna B. Lymphedema. 2020. StatPearls Publishing. Pubmed
13. The diagnosis and treatment of peripheral edema: 2016 Concensus Document of the International Society of Lymphology 2016; 49:170. Pubmed
14. Pereira de Godoy JM, Pereira de Godoy HJ, Sene Souza AA, Filho RB, Godoy FG. Lipolymphedema associated with Idiopathic cyclic edema: A therapeutic approach. 2017. Hindawi. CrossRef Pubmed
15. Mehrara BJ, Greene AK. Lymphedema and Obesity: Is there a link? 2014. Plast Reconstr Surg. American Society of Plastic Surgeons. CrossRef Pubmed
16. Brice G, Child AH, Evans A, Mansour S, Burnand K, Sarfarazi M, et al. Milroy disease and VEGFR-3 mutation phenotype. 2004. J Med.Genet. CrossRef Pubmed
17. Mahram M, Rajabi M. Treatment of Lymphedema Preacox through Low level laser therapy. 2011. Journal of Research in medical sciences. Pubmed
18. Pereira de Godoy JM, Rio A. Garcia PD, Guerreiro Godoy MF. Lymphedema in Klippel-Trenanunay Syndrome: Is it possible to normalize.2016. Hindawi Publishing Corporation. CrossRef Pubmed
19. Ibrahim A. Primary lymphedema tarda. 2014. Pan Afr Med. 19:16. CrossRef Pubmed
20. Goss JA, Maclallan RA, Green AK. Resolution of Primary Lymphedema: A case report. Plastic Reconstr Surg Glob Open. 2017 Feb; 5(2):e1223. CrossRef Pubmed
21. Ribeiro Pereira ACP, Koifman RJ, Bergmann A. Incidence and risk factors of lymphedema after breast cancer treatment: 10 years of follow-up. 2017. Pubmed Breast. Dec;36:67-73. CrossRef Pubmed
22. Farrow W. Phlebolymphedema- A common underdiagnosed and undertreated problem in the wound care clinic. 2010. Journal of the American College of Certified Wound Specialists 2, 14–23. CrossRef Pubmed
23. Kron, M, Walker E, Hernandez L, Torres E, Libranda-Ramirez, B. Lymphatic Filariasis in the Philippines. 2000. Parasitology Today. 16(8), 329–333. CrossRef Pubmed
24. Bosman J. Lipoedema: Poor knowledge, neglect or disinterest. 2011. Journal of lymphoedema. Vol 6. No. 2.
25. Johnson KC, Kennedy AG, Henry SM. Clinical measures of lymphedema. 2014. Lymphatic research and biology. Volume 12 Number 4. CrossRef Pubmed
26. Gutknecht M, Herberger K, Klose K, Purwins S, Dietz D, Blome C, Augustin M. Cost-of-illness of patients with lymphoedema. J Eur Acad Dermatol Venereol. 2017 Nov;31(11):1930-1935. doi: 10.1111/jdv.14442. Epub 2017 Oct 10. PMID: 28662302. CrossRef Pubmed
27. Weiss R. Cost of a lymphedema treatment mandate-10 years of experience in the Commonwealth of Virginia. Health Econ Rev. 2016 Dec;6(1):42. doi: 10.1186/s13561-016-0117-3. Epub 2016 Sep 2. Erratum in: Health Econ Rev. 2016 Dec;6(1):47. PMID: 27590738; PMCID: PMC5010541. CrossRef Pubmed
Copyright Information
