Original Article
Aug 2022, 31:1
First online: 3 August 2022
Original Article
Normal Weight Central Obesity among Filipinos and Its Association with Cardiovascular Risk: A Cross-Sectional Study
Bryan Rene F. Toledano MD,1 Emily Mae L. Yap M.D,2 Gerald C. Vilela M.D 2
Main Author: Bryan Rene F. Toledano, MD
Email: imbryantoledano@gmail.com, phcresearch@gmail.com
Contact number: 09054776260
ABSTRACT
INTRODUCTION
The study aims to measure the prevalence of normal-weight central obesity, to measure its association with cardiovascular risks and diseases and to compare it across the different subtypes of obesity among Filipinos.
METHODS
The participants were Filipinos age 20 years old above who had participated and completed the desired data in the National Nutrition Survey II. The participants were categorized into the following groups: normal weight (BMI 18.5–24.9 kg/m2) and no central obesity; normal weight with central obesity (WC ≥ 80cm or WHR ≥ 0.85 for females, WC ≥ 90cm or WHR ≥ 0.90 for males); overweight (BMI ≥25-29.9kg/m2); overweight with central obesity; obese (BMI ≥30kg/m2) and obese with central obesity (OBCO). A Binary logistic regression was utilized to determine the odds ratio (OR) and 95% confidence intervals (CI) for hypertension, diabetes, and dyslipidemia.
RESULTS
A total of 5,920 participants (2,883 men and 3,037 women) were analyzed. The prevalence of normal weight central obesity was 39.3%. In comparison to normal weight, the ORs for hypertension
(OR=1.84, p=0.001), diabetes (OR=2.1, p=.001), dyslipidemia (OR=1.3, p=.002), in Obese with central obesity for hypertension (OR=2.2, p=.001), diabetes (OR=2.7, p=.001), dyslipidemia (OR=1.29, p=.10) and in Overweight with central obesity hypertension (OR=1.65, p=.001), diabetes (OR=1.58, p=.001), dyslipidemia (OR 1.28, p=.004) were significantly higher in Normal weight central obesity.
CONCLUSION
Normal weight central obesity is a common finding among Filipinos and is associated with greater cardiovascular risks of hypertension, diabetes, or dyslipidemia in comparison with obese and overweight.
KEYWORDS
normal weight central obesity, Filipinos, obesity paradox
INTRODUCTION
Obesity is a modifiable risk factor that is defined as excess body fat associated with increased morbidity and mortality.1 It is a public health problem that needs attention and early identification. There have been several efforts to measure obesity and its application to screening large populations. The most widely used are body mass index (BMI) and central obesity (CO). Traditionally the correlation is positive, the higher the BMI and CO the greater the risk of cardiovascular disease and death.2, 3, 4, 5, 6, 7 In a local study done by Sy. et al, using the National Nutrition and Health survey last 2008, obesity among Filipinos had a prevalence of 4.9% when measured by BMI while CO is 10.2% in men and 65.6% in women when measured by the waist-hip ratio (WHR).2 There has been conflicting data, that suggests the obesity paradox, showing that some overweight or obese patients have lower cardiovascular risk while others with normal BMI have increased risk.8, 9 The possible explanation is the concept of normal weight central obesity (NWCO), in which certain ethnicity like Asians tend to have increased fat mass compared to low lean mass with the same BMI and that CO is a better predictor for cardiovascular morbidity and mortality.10, 11 In light of this, many countries have done prevalence studies regarding NWCO, taking into account the BMI and CO using waist circumference (WC), waist to hip ratio (WHR), or waist to height ratio to raise awareness regarding its higher association with hypertension, diabetes, dyslipidemia, and coronary artery disease.12, 13, 14, 15, 16 New studies have also found that NWCO may confer the highest long-term risk of major adverse clinical events leading to mortality in patients with hypertension and coronary artery disease.17, 18, 19, 20
The study aims to measure the prevalence of normal normal weight central obesity, its association with cardiovascular risk and to compare it across the different subtypes of obesity among Filipinos. The information would be useful to raise awareness and plan potential interventions.
OBJECTIVES
- To determine the prevalence of Filipinos with normal weight central obesity
- To compare the associated cardiovascular risks of Filipinos with and without central obesity
- To compare the associated cardiovascular risks of Filipinos with normal weight central obesity and across the different subtypes of obesity
METHODOLOGY
We conducted a cross-sectional study using the data from the National Nutrition and Health Survey in 2008 (NNHeS II). It was obtained from The Department of Science and Technology- Food and Nutrition Research Institute (DOST-FNRI). The NNHeS II employed a stratified multistage sampling that covered the entire Philippine population of adults aged 20 years old and above. Sampling was done at the barangay/community, enumeration areas, and household levels from the 17 regions of the country. The population that represented the whole country was generated by sampling 25% of those households. The data requested are measures of blood pressure, anthropometrics of height, weight, WC, WHR, BMI, the medical information of cardiovascular diseases of hypertension, diabetes, dyslipidemia, coronary artery disease, cerebrovascular disease, and peripheral arterial disease. The participants with complete data as stated were used, categorized, and analyzed. This study has been approved by the DOST-FNRI and Institutional Ethical Review Board of The Philippine Heart Center. A detailed description of the survey design and procedures has been published last 2012.7
Operational definitions7
- Body mass index – calculated as the weight in kilograms divided by the square of the height in meters, categories are: underweight (<18.5 kg/m2), normal (18.5-24.9 kg/m2), overweight (25-29.9 kg/m2), obese (>/=30 kg/m2).
- Hypertension – systolic BP (SBP) of 140 mm Hg or higher, diastolic BP (DBP) of 90 mm Hg or higher while using the mean of 3 measurements during a single visit, a previous diagnosis of hypertension, or use of antihypertensive medication
- Diabetes Mellitus – fasting plasma glucose level of 7.0 mmol/L (126 mg/dL) or higher, or a history of diabetes, with or without the use of oral antihyperglycemic medication or insulin.
- Dyslipidemia – any abnormalities from the lipid profile as high total cholesterol >/=6.20mmol/L (240 mg/dL), high LDL-C >/=4.14 mmol/L (160 mg/dL), high TG and >/=2.26 mmol/L (200 mg/dL), Low HDL-C </= 1.03 mmol/L (40 mg/ dL) (20), with or without the use of anti dyslipidemia medications.
- Coronary artery disease (CAD) – previous heart attack, or documented ischemia or coronary artery occlusive disease diagnosed by a medical doctor or a nurse
- Cerebrovascular accident (CVA) – previous stroke or transient ischemic attack diagnosed by a medical doctor or a nurse
- Peripheral arterial disease (PAD) – previously diagnosed occlusive disease by a medical doctor or a nurse
- Waist circumference – measured at the midpoint between the lowest rib and the iliac crest by a field worker with comprehensive training
- Hip circumference measured at the greater trochanter or widest diameter of the hips by a field worker with comprehensive training
- Central Obesity – waist-hip ratio (WHR) >/= 0.85 women, >/= 0.90 men or waist circumference (WC) >/= 80 women and >/= 90 men
Data organization, editing, processing, and analysis
The data obtained were checked for completeness and categorized into 8 subtypes using Microsoft Excel (version 16.30): 1. Underweight (UW), 2. Underweight with central obesity (UWCO), 3. Normal weight (NW), 4. NWCO, 5. Overweight (OW), 6. Overweight with central obesity (OWCO), 7. Obese (OB) and 8. Obese with central obesity (OBCO). The rechecking of data was done twice to ensure correctness and validity.
Statistical Analysis
All analyses were performed using the Statistical Package for the Social Sciences (version 20, with license) and MEDCALC version 10 (with license). The univariate analysis includes independent samples T-test for continuous variables and Chi-Square for categorical outcomes. Binary logistic regression using forward technique was utilized to determine the significant correlates for each risk factor/cardiovascular outcome. Odds ratios above 1, with p-values less than 05 indicated an association with the outcome. Adjustment for potential confounding variables was done using the Mantel-Haenszel test. Mean differences were determined using an independent T-test between obesity categories. Precision estimates were pegged at 95% confidence level.RESULTS
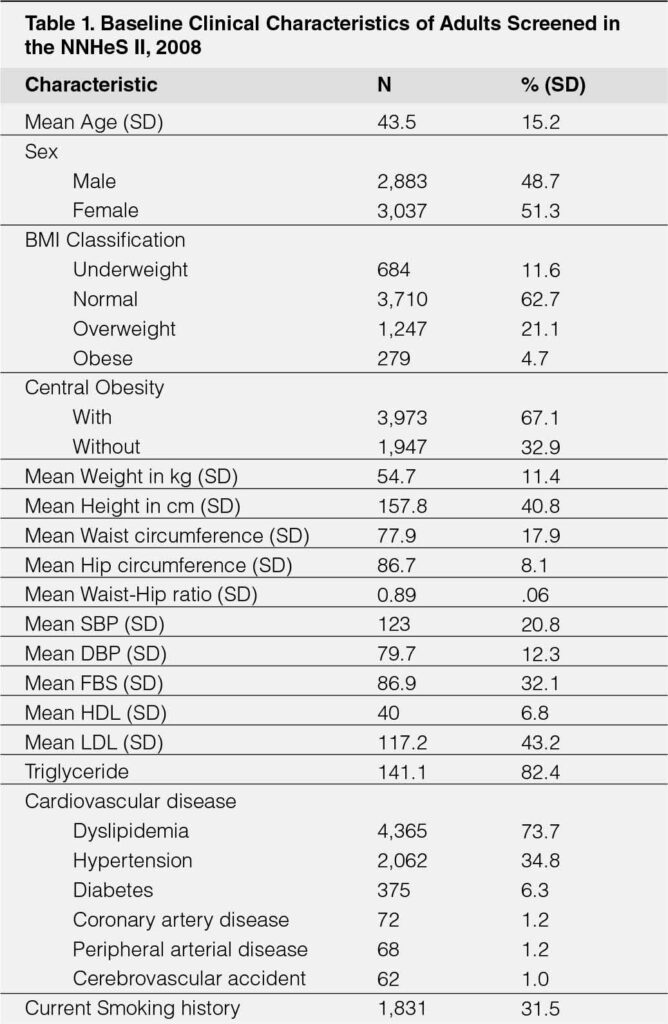
The analysis included a total of 5,920 adult individuals with desired variables as screened from the National Nutrition and Health Survey II. Their baseline clinical characteristics are summarized. (Table-1). The mean age was 43.5 (± 15.2) years, with slight female predominance (51.3% versus 48.7%). As to Body Mass Index classification, 11.6% were categorized as underweight, 62.7% as normal, 21.1% as overweight and 4.7% as obese. The occurrence of central obesity across the BMI categories is also depicted. (See also Table-2) The average values for height, weight, systolic and diastolic pressures, lipid profile (HDL, LDL, and triglycerides) are recorded.
Among the cardiovascular disease risk and diseases, dyslipidemia was present in 73.7%, followed by hypertension (34.8%), diabetes (6.3%), coronary artery disease (1.2%), peripheral arterial occlusive disease (1.2%) and cerebrovascular disease (1.0%). Current smokers at the time of the study were reported in 31.5%.
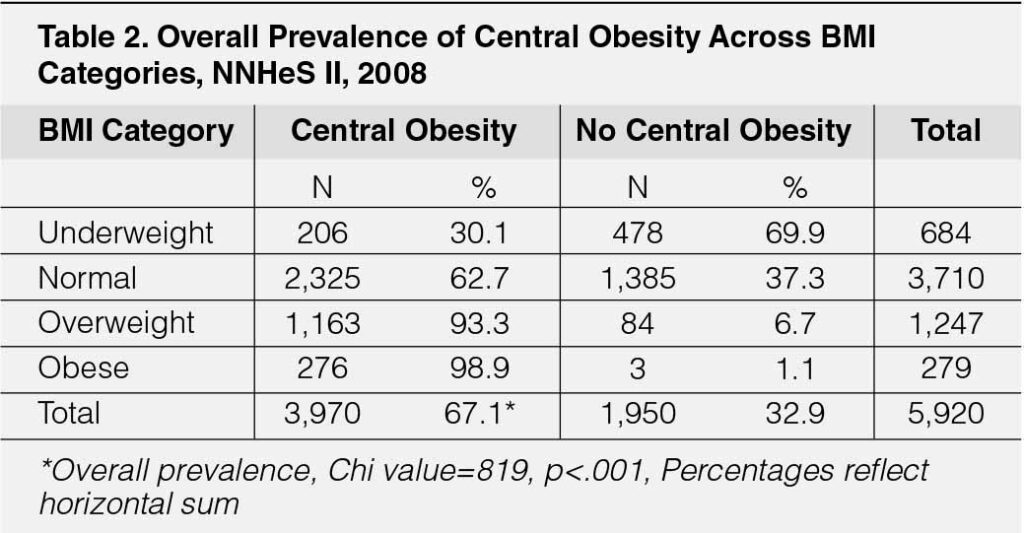
The prevalence of central obesity (regardless of BMI category) was 67.1% (3,973 out of 5,920) while the prevalence of normal weight central obesity in this study was 39.2% (or 2,325 out of 5,920). Those who were obese had the highest prevalence of central obesity (98.9%) followed by those who were overweight (93.3%). The prevalence of central weight obesity among those with “normal BMI” is 62.7% (2,325 out of 3,710) which was statistically higher among the underweight (30.1%) (p<.001) (Table-2).
COMPARISON OF CARDIOVASCULAR DISEASE AND RISK FACTORS IN CENTRAL OBESITY ACROSS BMI CATEGORIES
ACROSS ALL BMI CATEGORIES
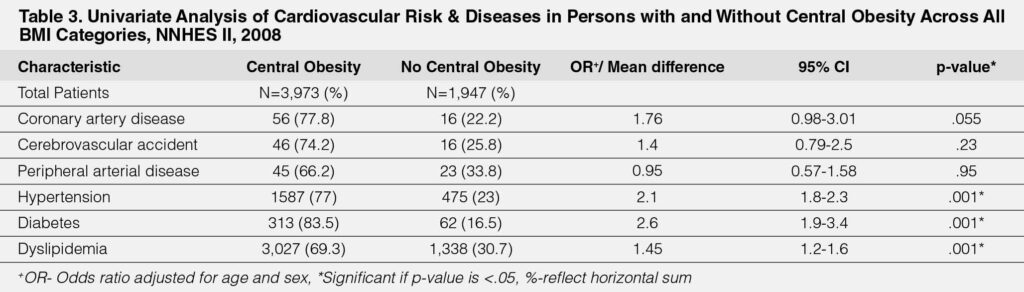
Table-3 displays the overall comparison of risk factors and cardiovascular conditions among those with and without central obesity across all BMI categories. Adjusting for age and sex, those with central obesity were at high risk for hypertension (OR 2.1, 95% CI 1.8,2.3, p<.001), thrice the risk for diabetes (OR 2.6, 95% CI 1.9-3.4, p<.001) and almost twice the risk for dyslipidemia (OR 1.45, 95% CI 1.2-1.6, p<.001).
NORMAL WEIGHT CATEGORY
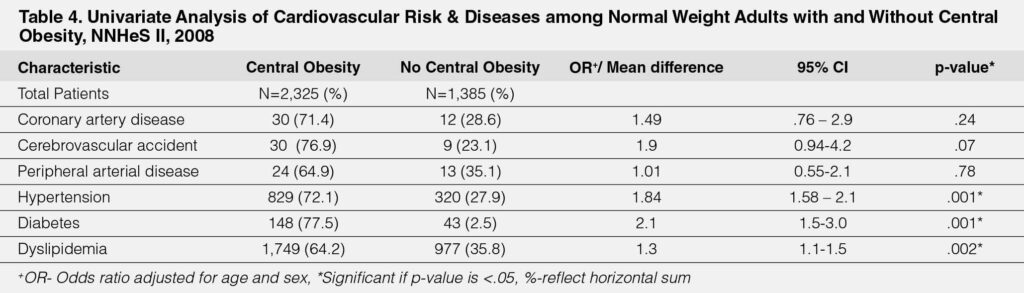
Those with normal weight with central obesity were at higher risk for hypertension (OR=1.84, 95% CI, 1.58-2.1, p=.001); a higher
risk for diabetes (OR=2.1, 95% CI 1.5-3.0, p=.001); higher risk for dyslipidemia (OR=1.3, 95% CI 1.1-1.5, p=.002) compared to
those who had normal weight without central obesity. (Table-4)
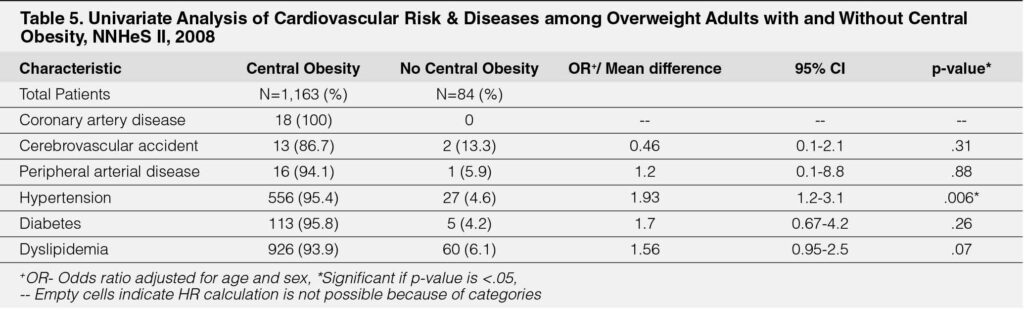
OVERWEIGHT CATEGORY
Those who were overweight with central obesity had twice the risk for hypertension when compared to their counterparts without central obesity (OR-1.93, 95% CI 1.2-3.1, p=.006). (Table-5).
COMPARISON OF CLINICAL CHARACTERISTICS ACROSS DIFFERENT SUBTYPES OF OBESITY
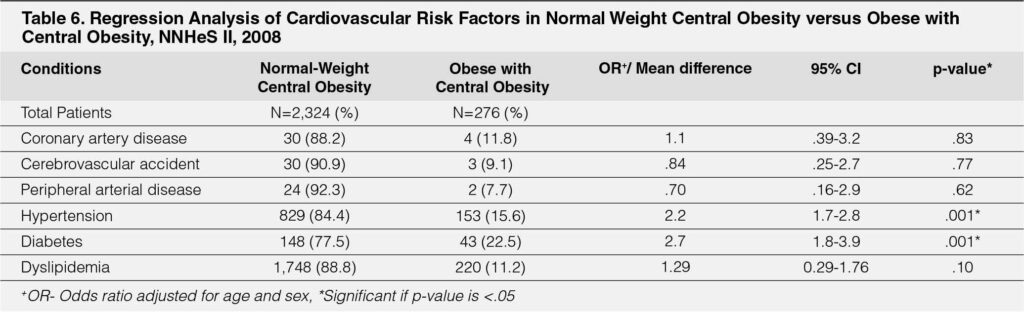
Normal Weight Central Obesity versus Obese with Central Obesity
After adjusting for age and sex, adults with normal weight central obesity had a two-fold risk of hypertension (OR=2.2, 95% CI 1.7,2.8, p<.001), almost thrice the risk for diabetes (OR 2.7, 95% CI 1.8,3.9, p<.001). There was no difference in the risk for dyslipidemia. (Table-6).
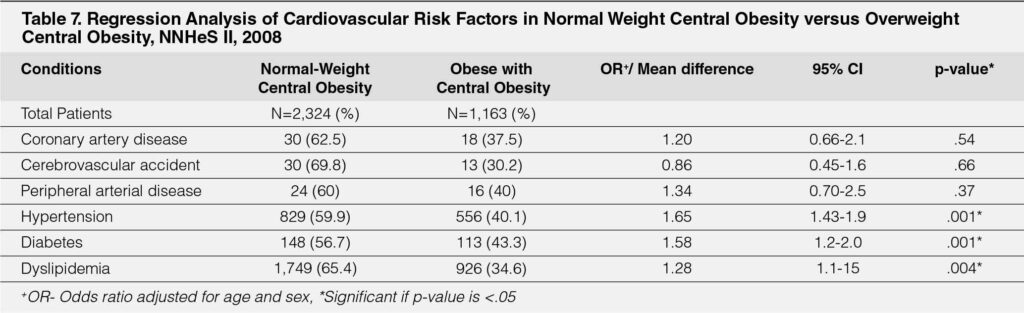
Normal Weight Central Obesity versus Overweight Central Obesity
When compared to those who were overweight with central obesity, patients who were with normal weight with central obesity had almost twice the risk of hypertension (OR=1.65, 95% CI 1.43-1.9, p=.001) and diabetes (OR=1.58, 95% CI 1.2-2.0, p=.001) were dyslipidemia (OR 1.28, 95% CI 1.1-1.5, p=.004). (Table-7). There was no observable higher risk for coronary artery disease (CAD), cerebrovascular disease (CVD) and peripheral arterial disease between the two types of central obesity.
DISCUSSION
A total of 5,920 from 7,700 participants that have complete variables were included and analyzed. This difference reflects the slight variations in the prevalence of some of the outcomes reported. In the previous study2 that used the same NNHeS 2008 survey, the obese by BMI is 4.9% compared to 4.7%, CO 75.8% to 67.1% Hypertension 24.6% to 34.8%, Diabetes 5.2% to 6.3%, Dyslipidemia 72% to 73.1%, Smoker 31% to 31.5%, CAD 1.1% to 1.2%, CVA .9% to 1% and PAD 1.0% to 1.2% based on our study. There were no associations seen in CAD, CVA, and PAD probably because of the low event rates. The latest NHHeS in our country done last 2013 showed an increasing trend of overweight and obese combined using BMI of 31.1% from 25.8%, however, our study tallied a slightly higher prevalence of central obesity of 67.1% from 63.2%.3
The higher prevalence of central obesity with increasing BMI can be partly explained by the percent of fat aside from lean mass and bone mass9 that comprise the total body weight. Hence the observation of inverse prevalence of CO in the normal weight and underweight group. In general, the study validated a higher risk for hypertension, diabetes, and dyslipidemia in all participants with CO specifically in NWCO compared to NW, and higher risk for hypertension in OWCO compared to OW. The result was consistent with previous studies showing the value of CO as a clinical marker of risk.12, 25, 26
This is the first local study among Filipinos that reported the prevalence of NWCO which is 39.3% and is higher compared to other cross-sectional studies done in different countries including Chile 2.4%,13 China 6.13%,14 USA 14.3%,18 Thailand 15.4%,15 Japan 19.9%16 and South Africa 36.9%.17 The difference in prevalence may be due to genetic, dietary, and physical activity variations. It is also important to note the possible contrasting sampling size, methodology, and how the operational definitions were used and measured.
The NWCO has a higher risk of hypertension and diabetes when compared to OBCO and hypertension, diabetes, and dyslipidemia when compared to OWCO. These results were also seen in other studies and were correlated with an increased risk of mortality in this group. Higher visceral fat and lower lean mass maybe the reason in this group and are associated with abnormalities in cardiometabolic such as insulin resistance, dyslipidemia and inflammation.18, 19, 23, 24
This present study suggests that categorizing obesity using the combination of BMI and CO and reporting NWCO would help identify patients with cardiovascular risk factors. Those with NWCO is a common finding and is associated with higher cardiovascular risk compared to other subtypes. The screening and identification of this group will increase awareness regarding the risks associated such as hypertension, diabetes, and dyslipidemia. A strategic approach of proper diet27, 28 and exercise39, 30 to prevent central obesity as measured by WC and WHR and to increase lean muscle mass to prevent NWCO, may decrease cardiovascular risks.
LIMITATIONS & RECOMMENDATIONS
There are several limitations of this study first it is a retrospective study that used the data done last 2008. A longitudinal study with long-term follow up would be necessary to establish if the cardiovascular risk seen in NWCO, will translate to cardiovascular diseases such as CAD, CVA, PAD, and mortality. Second, the category of a participant was based on a certain point and may vary with time, these possible changes were not accounted for. Third, an operational definition using the Asian BMI cut off would have increased the prevalence of NWCO and may be used in reporting for our national survey. Fourth, obesity subtypes such as obese and overweight without central obesity are uncommon which made the sample size small and underpowered to generate any significant result. Finally, there are other imaging modalities to accurately identify the amount of visceral fat and lean muscle mass of a participant such as dual-energy X-ray absorptiometry. However, this is not feasible for mass screening and our lack of resources.
CONCLUSION
In conclusion, the present study showed that NWCO is a common finding among Filipinos and is associated with greater CVD risks such as hypertension, diabetes, and dyslipidemia in comparison with obese and overweight.
REFERENCES
1. Mann DL, Zipes DP, Libby P, Bonow RO, and Braunwald, E. Braunwald’s heart disease: A textbook of cardiovascular medicine (Eleventh edition). 2015. Philidelphia, PA: Elesevier/Saunders.
2. World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1-452. Pubmed
3. Food and Nutrition Research Institute-Department of Science and Technology (FNRI-DOST). (2015). Philippine Nutrition Facts and Figures 2013: 8th National Nutrition Survey Overview. FNRI Bldg., DOST Compound, Bicutan, Taguig City, Metro Manila, Philippines.
4. WHO. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation. WHO Technical Report Series 894. Geneva: World Health Organization. 2000. Pubmed
5. Mathieu P, Poirier P, Pibarot P, Lemieux I, Despres JP. Visceral obesity: the link among inflammation, hypertension, and cardiovascular disease. Hypertension. 2009;53:577-584. CrossRef Pubmed
6. NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults – The Evidence Report. National Institute of Health. 1998. Obesity research, 6 Suppl 2, 51S-209S.
7. Sy RG, Morales DD, Dans AL, Paz-Pacheco E, Punzalan FR, Abelardo NS, and Duante CA. Prevalence of atherosclerosis-related risk factors and disease in the Philippines. 2012. J Epidemiology. 22(5):440-447. CrossRef Pubmed
8. Ashwell M, and Gibson S. Waist to height ratio is simple and effective obesity screening tool for cardiovascular risk factors: analysis data from the British national diet and nutrition survey of adults aged 19-64 years. 2009. The European journal of obesity. 2:97-103. CrossRef Pubmed
9. Bluher M. The distinction of metabolically “healthy from unhealthy” obese individuals. Curr Opin Lipidol. 2010:21:38-43. CrossRef Pubmed
10. Cornier MA, Després JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, Lopez-Jimenez F, Rao G, St-Onge MP, Towfighi A, Poirier P; American Heart Association Obesity Committee of the Council on Nutrition; Physical Activity and Metabolism; Council on Arteriosclerosis; Thrombosis and Vascular Biology; Council on Cardiovascular Disease in the Young; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing, Council on Epidemiology and Prevention; Council on the Kidney in Cardiovascular Disease, and Stroke Council. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011 Nov 1;124(18):1996-2019. doi: 10.1161/CIR.0b013e318233bc6a. Epub 2011 Sep 26. PMID: 21947291. CrossRef Pubmed
11. Oliveros E, Somers VK, Sochor O, Goel K, and Jimenez FL. The concept of normal weight obesity. 2014. Progress in cardiovascular disease; 56: 426-433. CrossRef Pubmed
12. Prasad DS, Kabir Z, Dash AK, and Das BC. Abdominal Obesity an independent cardiovascular risk factor. In Indian subcontinent: A clinic epidemiologic evidence summary. J Cardiovasc Dis Res 2011;2:199-205. Pubmed
13. Villanueva B, Arteaga A, Maiz A, and Cortes B. Abdominal obesity is a common finding in normal weight subjects in Chile and is associated with increased frequency of cardiometabolic risk factors. PLOS ONE 13(3). CrossRef Pubmed
14. Zhang P, Wang R, Gao C, Jiang L, Lv Xin, Song Y and Li Bo. Prevalence of central obesity among adults with normal BMI and its association with metabolic disease northeast china. PLoS ONE 11(7). CrossRef Pubmed
15. Thaikruea L, and Thammasarot J. Prevalence of normal weight central obesity among Thai health care providers and their association with CVD risk: a cross sectional study. Scientific reports. 6:371000. CrossRef Pubmed
16. Shirasawa T, Ochiai H, Yoshimoto T, Nagahama S, Kobayashi M Ohtsu I, Sunaga
Y, and Kokaze A. Associations between normal weight central obesity and cardiovascular disease risk factors in Japanese middle-aged adults: a cross sectional study. 2019. Journal of Health, Population and Nutrition. BMC. 38:46. CrossRef Pubmed
17. Owolabi EO, Goon DT, and Adeniyi OV. Central obesity and normal weight central obesity among adults attending healthcare facilities in Buffalo City Metropolitan Municipality. South Africa: a cross sectional study. Journal of health, population and nutrition. 2017. CrossRef Pubmed
18. Sahakyan K, Somers V, Escudero JR, Thomas R, Sochor O, Singh P, and Jimenez FL. Normal weight central obesity and cardiovascular mortality risk in hypertensive patients. 2013. JACC. V16 I10.
19. Sharma S, Batsis JA, Coutinho T, Somers VK, Kragelund C, Kanaya AM, and Jimenez FL. Normal weight obesity is associated with the highest mortality risk in older adults with coronary artery disease. 2015. Journal of clinical lipidology vol 9 no. 3.
20. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, Jones DW, Materson BJ, Oparil S, Wright Jr JT, and Roccella EJ. National Heart, Lung and Blood Institute Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure: National High Blood Pressure Education Program Coordinating Committee. 2003. JAMA. CrossRef Pubmed
21. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285(19):2486–97. CrossRef Pubmed
22. Waist circumference and waist–hip ratio: report of a WHO expert consultation, Geneva, 8–11 December 2008.
23. Sahakyan KR, Somers VK, Rodriguez-Escudero JP, Hodge DO, Carter RE, Sochor O, Coutinho T, Jensen MD, Roger VL, Singh P, and Lopez-Jimenez F. Normal weight central obesity: Implications for total and cardiovascular mortality. 2016. Ann Internal Med 163(11): 827-835. CrossRef Pubmed
24. Bosomworth N.J. Normal weight central obesity: Unique hazard of the toxic waist. 2019. Canadian Family Physician. June Vol 65. Pubmed
25. Mathieu P, Poirier P, Pibarot P, Lemieux I, Despres JP. Visceral obesity: the link among inflammation, hypertension, and cardiovascular disease. Hypertension. 2009;53:577-584. CrossRef Pubmed
26. Fan H, Li X, Zheng L, Chen X, Lan Q, Wu H, Ding X, Qian D, Shen Y, Yu Z, Fan L, Chen M, Tomlinson B, Chan P, Zhang Y, Liu Z. Abdominal obesity is strongly associated with Cardiovascular Disease and its Risk Factors in Elderly and very Elderly Community-dwelling Chinese. Sci Rep. 2016 Feb 17;6:21521. doi: 10.1038/srep21521. PMID: 26882876; PMCID: PMC4756331. CrossRef Pubmed
27. Kesztyüs D, Erhardt J, Schönsteiner D, Kesztyüs T. Therapeutic Treatment for Abdominal Obesity in Adults. Dtsch Arztebl Int. 2018 Jul 23;115(29-30):487-493. doi: 10.3238/arztebl.2018.0487. PMID: 30135008; PMCID: PMC6121087. CrossRef Pubmed
28. Watson RR. Nutrition in the prevention and treatment of Abdominal Obesity. 2014. Elsevier.
29. Slentz CA, Houmard JA, and Kraus WE. Exercise, Adbominal Obesity, Skeletal, Muscle and Metabolic Risk: Evidence for a Dose Response 2009. 17(03):S27- S33. CrossRef Pubmed
30. Koros MC. DOH’S Belly Good for Health Program as a Strategy to Improve the Body Mass Index (BMI), Waist Circumference and Blood Pressure among Overweight and Obese Municipal Employees of Mahayag, Zamboanga Del Sur. 2016. Health Research and Development Information Network. R09- ADZU-17050511260381.
Copyright Information
