Original Article
July 2023, 32:2
First online: 9 July 2023
Original Article
Left Ventricular Global Longitudinal Strain as a Predictor for Poor Outcomes in Patients Hospitalized for COVID-19 Infection
Juan Armando D. Diaz, M.D, 1 Raul L. Lapitan, M.D 2
2 Makati Medical Center, Philippine College of Physicians, Philippine College of Cardiology, American College of Cardiology. E-mail: Raul.lapitan522@gmail.com
ABSTRACT
BACKGROUND
Establishing a correlation between left ventricular global longitudinal strain (LV-GLS) with transthoracic echocardiography (TTE), and the severity and outcomes of patients infected with COVID-19 offers several advantages in patient care and management. This study aims to explore the utility of measuring the LV-GLS to predict outcomes in hospitalized patients infected with COVID-19.
METHODS
This was a retrospective cohort study of COVID-19 patients in a tertiary care center who had a TTE with GLS measurements from April 2021 to May 2021. Comparisons between parameters of left ventricular function (GLS and LVEF) were performed using the t-test or Mann-Whitney U test for continuous variables and the χ2 test or Fisher exact test for categorical variables. Kaplan-Meier survival analysis was used to estimate mortality and length of hospital stay. Log-rank test was used to assess the association of GLS on in-hospital mortality.
RESULTS
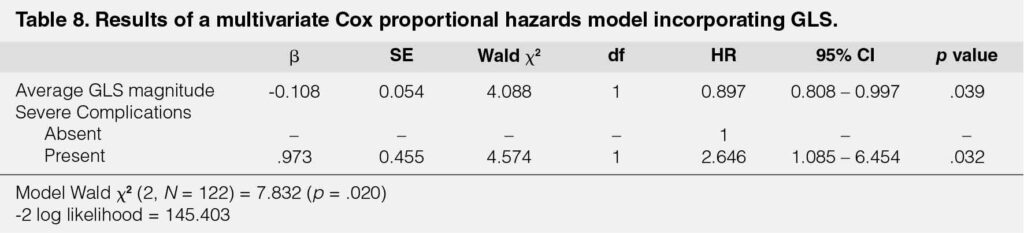
A total of 124 participants were included in the study. 73.2% (90/123) had a decreased GLS; average GLS was -19.2% [-27.6 to -4.7]. A significant model was created using GLS as a main factor with pre-selected co-variates with a Wald χ2 (2, N = 121) = 7.932 (p = .020). Co-variates were average GLS magnitude (HR = 0.897 [95% CI 0.808 to 0.997], p = .0.043) and presence of severe complications (HR = 2.630 [95% CI of 1.087 to 6.362], p = 0.032).
CONCLUSION
A model considering severe complications showed that among patients admitted for COVID-19 an abnormal average global longitudinal strain predicts increased in-hospital mortality.
INTRODUCTION
The COVID-19 pandemic has continued to affect the world since it was declared by the WHO in March, 2021. The causative agent, Severe acute respiratory coronavirus 2 (SARS-COV-2) has been spreading around the globe and undergone several mutations since it was first discovered. In the Philippines alone, there have been a total of 1, 165, 155 cases as of this writing, with 163, 869, 893 cases worldwide.1
The transthoracic echocardiogram (TTE) has been used extensively prior to the pandemic but has raised concerns about the safety of its performance on COVID-19 patients and leading to guidelines and recommendations for its use during this time.4-6 The global longitudinal strain can be done with a TTE and tracks individual points, called speckles, within an echo image, and measures the change in length of the myocardium between end diastole and end systole describing increases and decreases in strain. Global longitudinal strain (GLS) of the left ventricle can thus quantify myocardial function.7, 8 Establishing the utility of the transthoracic echocardiogram, particularly the global longitudinal strain, in correlating with severity and outcomes of patients infected with COVID-19 will allow for improved triaging of patients and, as the need arises, for the proper allocation of scarce resources. The global longitudinal strain may be documented faster than the release of some of the biomarkers available thus facilitating the clinician’s decision-making. The study aims to determine the relationship between global longitudinal strain and left ventricular ejection fraction (LVEF) with in-hospital mortality of patients diagnosed with COVID-19 at Makati Medical Center.
METHODS
Design, setting, and participants
This was a retrospective cohort study of COVID-19 patients in a tertiary care center (Makati Medical Center, Metro Manila, Philippines) who had a TTE with GLS measurements from April 2021 to May 2021 was done. Participants were included if they were (1) at least 18 years of age, (2) diagnosed with an active COVID-19 infection with a positive RT-Polymerase Chain Reaction nasopharyngeal and throat swab, (3) admitted and treated as inpatients, and (4) subject to a transthoracic 2D echocardiogram (TTE) done between April 1, 2021 to May 30, 2021 at Makati Medical Center. Participants were excluded if they were (1) less than 18 years of age, (2) no TTE, and (3) transferred to another hospital for any reason. COVID-19 severity was based on the discharge diagnosis based on the Philippine department of health Interim Guidelines on the COVID-19 disease severity, classification and management.
We extracted routine data from the electronic medical records, including baseline patient characteristics, clinical presentation, diagnostics, disease course, treatment, and outcome. All patient data were entered anonymously into a web-based electronic form, only using a study identifier. The coding manual and key linking patient information was saved in a local protected file which was not available to the researchers performing data analysis.
Transthoracic Echocardiography
Transthoracic echocardiography (TTE) was done at bedside in COVID-19 specific cohorting location in the study patients at rest in the left lateral decubitus, supine or sometimes seated position, as tolerated, with a GE Vivid S70N 2D echocardiography machine. The same machine was used to acquire all the images used in the study. Comprehensive transthoracic echocardiograms were performed according to guidelines and views set by the American Society of Echocardiography which included chamber dimensions and quantification.8 The images and views were then reviewed offline on the machine left ventricular (LV) GLS was measured with a two-dimensional speckle tracking analysis on apical two-, three-, and four-chamber views using vendor specific software available on the GE Vivid S70N machine according to guidelines.7 The frame rate of the two-dimensional echocardiographic data had been acquired 40 frames per second or higher. Left ventricular GLS measures the shortening of the myocardial fibers in the longitudinal direction and is conventionally presented as a negative value. Therefore, a less negative LV GLS (i.e., closer to 0) represents worse LV systolic function.
Clinical End Points and Outcomes
The outcome of interest in this study is in-hospital mortality. We defined in-hospital mortality as the occurrence of death within admission and was further described as the number of days from admission to death. Patients who were discharged home due to clinical improvement or transferred to a nursing home were considered recovered. Patients who were transferred to another hospital or were discharge with unknown reasons were considered censored. Length of hospital stay is defined as the number of days from patient to discharge.
Statistical analysis
The patients included in the study was presented using descriptive statistics. Categorical variables were presented as counts and percentages. Continuous variables were described using measures of central tendency depending on the normality of data.
Comparisons between parameters of left ventricular function (GLS and LVEF) were performed using the t test or Mann-Whitney U test for continuous variables and the χ2 test or Fisher exact test for categorical variables as appropriate. Kaplan-Meier survival analysis was used to estimate mortality and length of hospital stay. Pearson’s R was used to determine the association of parameters of left ventricular function with laboratory test results (Troponin I, D-dimer and NT-proBNP). Log-rank test was used to assess the association of GLS and EF on outcomes (mortality). Co-variates with known clinical significance were introduced into the statistical model. Collinearity diagnostics were done in the process. All tests were two-sided and p-values were considered significant when they are less than 0.05. Analysis was performed using SPSS version 26.0 statistical software.
Ethical considerations
This study was reviewed and approved by the Institutional Review Board and conducted in accordance with the ethical principles based on the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use-Good Clinical Practice ICH-GCP, Declaration of Helsinki and the National Guidelines for Biomedical Research of the National Ethics Committee (NEC) of the Philippines.RESULTS
Descriptive and Outcome Data
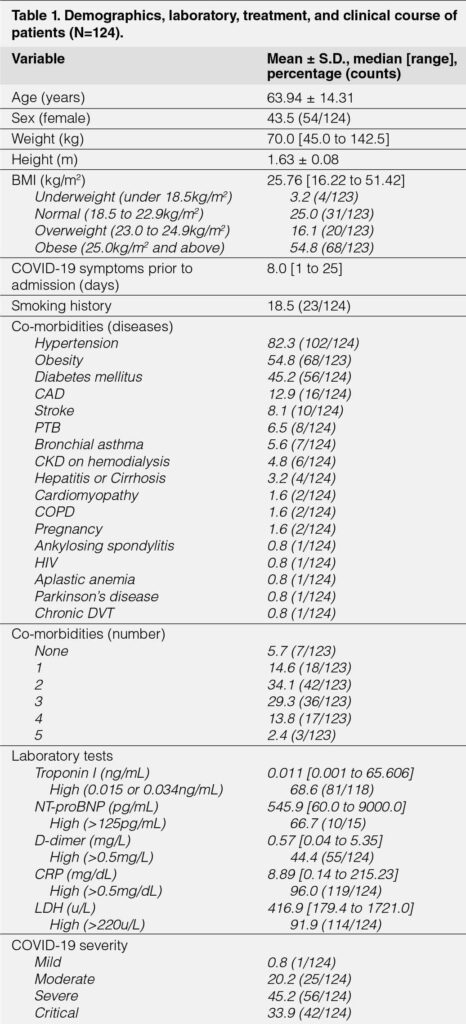
A total of 124 participants were included in the study. The average age was 63.9 ± 14.3 years with 43.5% being female (54/124). Average anthropometric measurements of height, weight, and body mass index (BMI) were 1.63 m (95% CI of 1.62 to 1.64), 70.0 kg [45.0 to 142.5], and 26.4 m2 [16.2 to 51.4]. Prior to admission, these patients experienced COVID-19 symptoms for eight days [1 to 25]. Smokers comprised 18.5% (23/124) of the sample. The most common co-morbidities were hypertension, obesity, and diabetes mellitus with percentages of 82.3% (102/124), 54.8% (68/123), and 45.2% (56/124), respectively. Majority (63.4%) had two to three co-morbidities (Table 1).
Laboratory tests retrieved included Troponin I, NT-proBNP, D-dimer, CRP, and LDH. Troponin I, D-dimer, CRP, and LDH were requested for majority of patients; while only 12.1% (15/124) had NT-proBNP results. Average values for Troponin I, NT-proBNP, D-dimer, CRP, and LDH were 0.011ng/mL [0.001 to 65.60], 545.9 pg/mL [60.0 to 9000.0], 0.57 mg/L [0.04 to 5.35], 8.89 mg/dL [0.14 to 215.23], and 416.9 [178.4 to 1721.0]. Majority of Troponin I, NT-proBNP, D-dimer, CRP, and LDH had high or abnormal results. (Table 1)
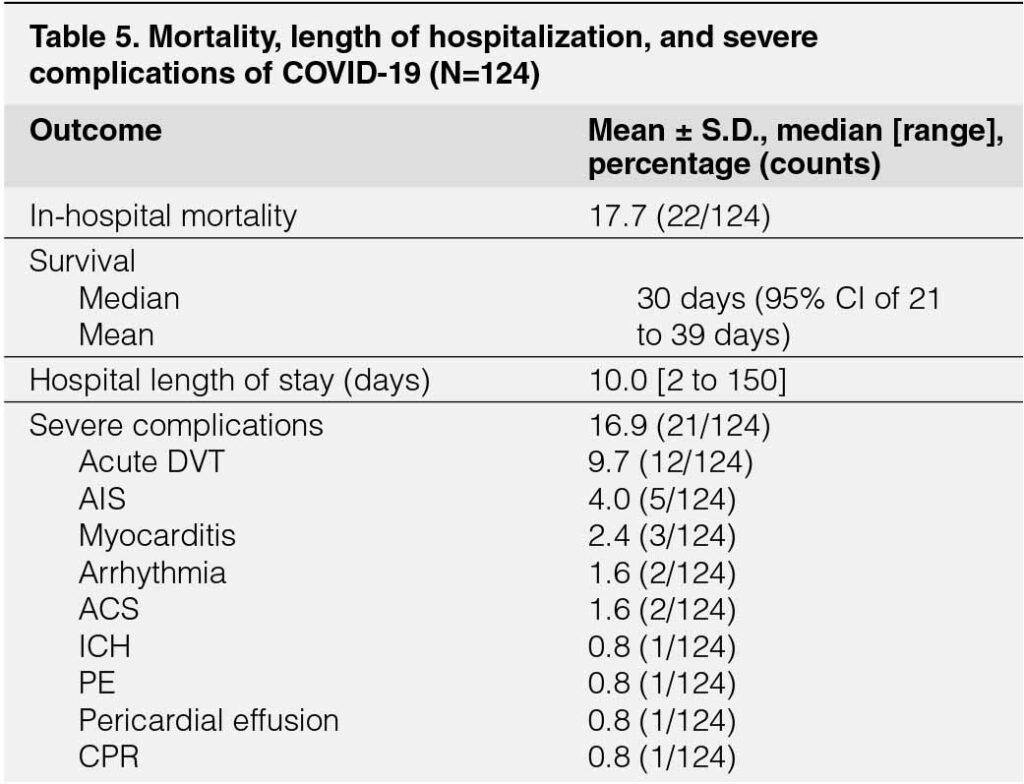
Most patients were diagnosed as severe (45.2%) or critical (33.9%) (Table 1 and Table 4) COVID-19. All patients received enoxaparin. Steroids were given to 86.3% (107/124). Remdesivir and Tocilizumab were respectively given to 96.0% (119/124) and 28.2% (35/124) patients. (Table 3) In the clinical course of patients, high-flow nasal oxygen, internal jugular vein catheter insertion, hemoperfusion, intubation, and inotropic support were given in 46.0%, 33.9%, 24.2%, 24.2%, 18.5% of patients respectively. (Table 3) Severe complications occurred in 16.9% (21/124) of patients; the most frequent were acute deep venous thrombosis, acute ischemic stroke, myocarditis, and arrhythmia in 16.9%, 9.7%, 4.0%, and 2.4%.
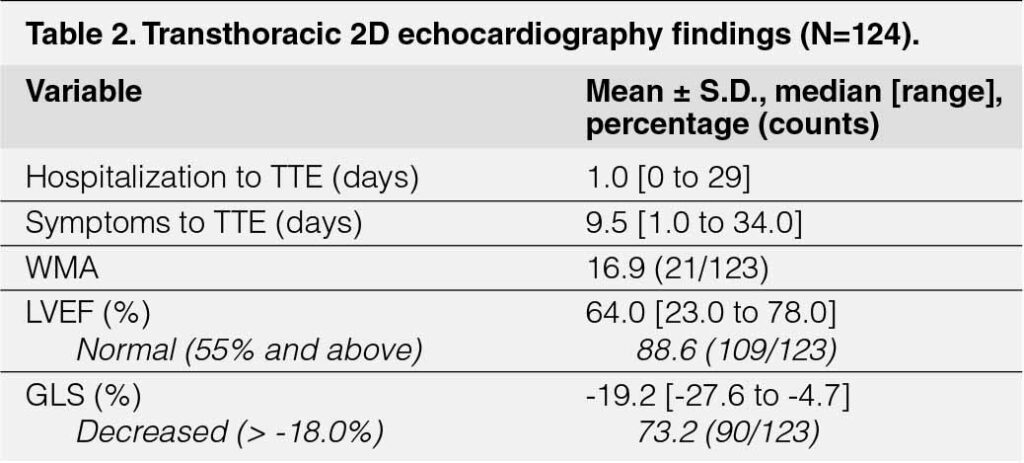
A total of 124 TTE’s were performed on an average of nine and a half days [1 to 34] and one day [0 to 29] from the start of COVID-19 symptoms. (Table 2) Most patients (88.6%) had a normal left ventricular ejection fraction with an average of 64% [23 to 78]. Wall motion abnormalities were seen in 16.9% (21/123). Majority 73.2% (90/123) had a decreased GLS; average GLS was -19.2% [-27.6 to -4.7]. A patient had a missing GLS result.

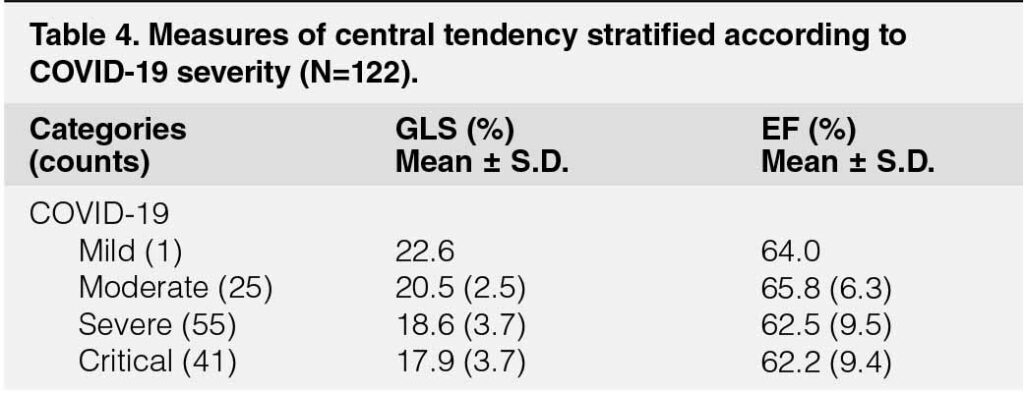
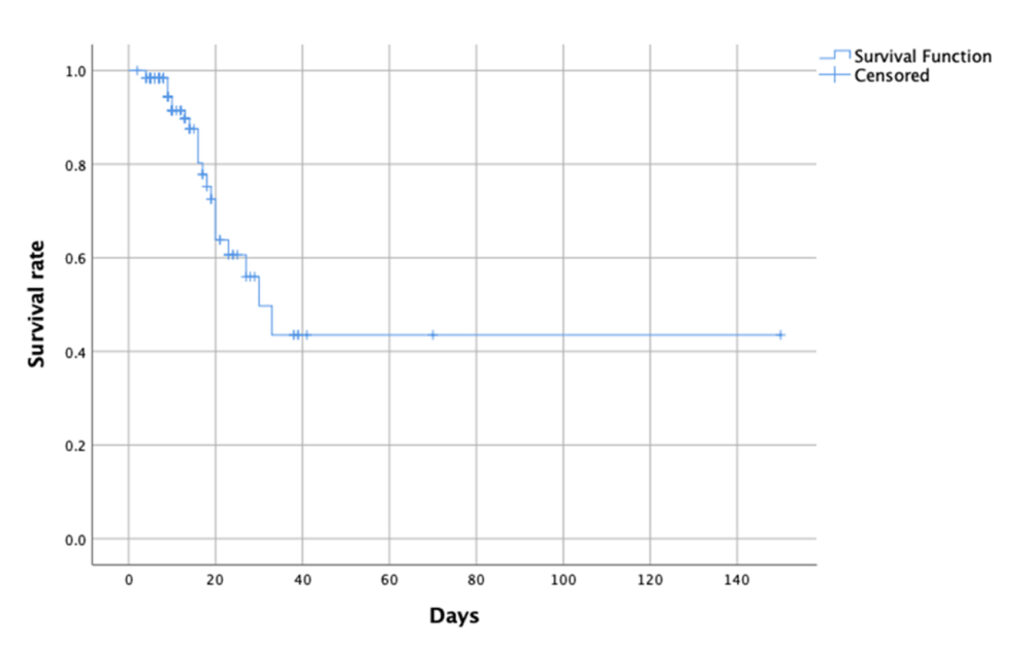
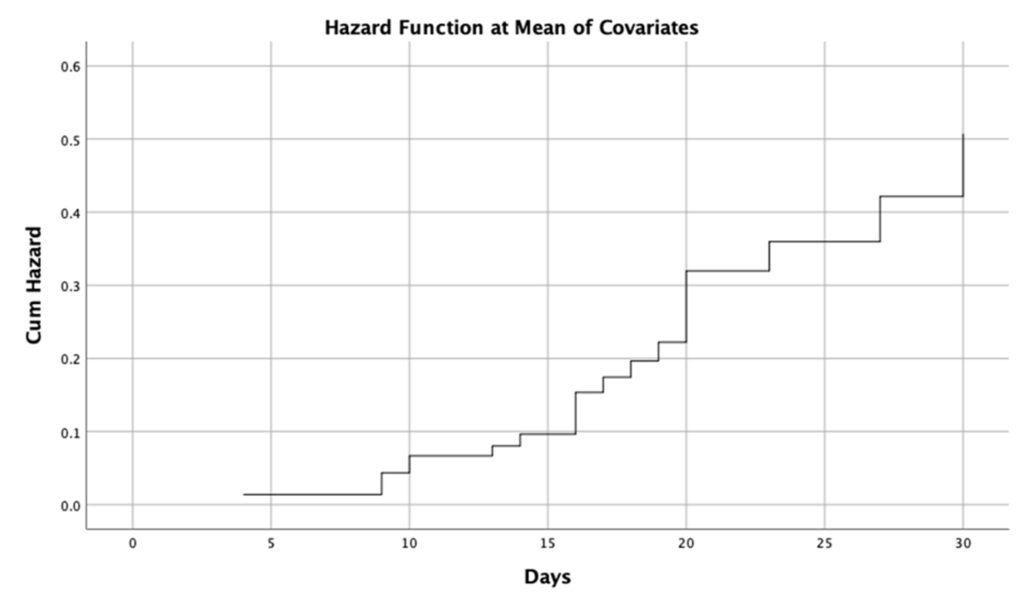
Majority of patients in the sample were discharged. The average length of hospitalization was ten days [2 to 150]. In our study, 17.7% (22/124) died while admitted at the hospital. (Table 5) In estimating the survival of our sample, in-hospital mortality and length of hospital stay are the event indicator and measure of time, respectively. A Kaplan-Meier survival curve was plotted (Figure 1); the median survival was 30 days (95%CI of 21.0 to 39.0 days) for our sample.
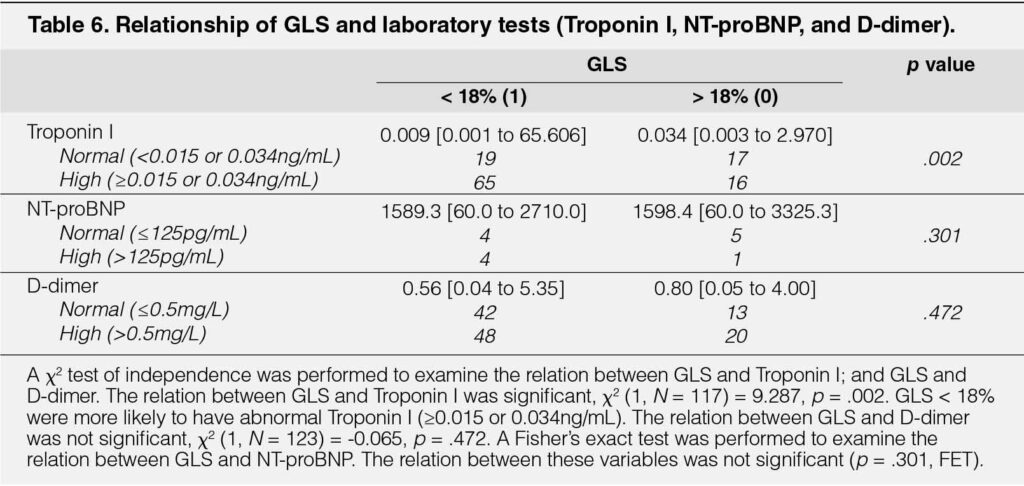
Association of LV Function and Laboratory Parameters
Clinically pertinent cut-offs for LV function (EF, GLS) and laboratory (Troponin I, NT-proBNP, D-dimer) were used. This is especially pertinent for the case of Troponin I where the result is laboratory dependent (e.g. a high Troponin I ≥0.015 or ≥0.034ng/ mL). A χ2 test of independence was performed to examine the relation between GLS and Troponin I; and GLS and D-dimer. The relation between GLS and Troponin I showed a χ2 value (1, N = 117) = 9.287, p = .002. GLS and D-dimer had a χ2 value (1, N = 123) = -0.065, p = .472. A Fisher’s exact test was performed to examine the relation between GLS and NT-proBNP with a p = .301, FET. (Table 6)
Association of LV Function Parameters with Outcomes
A clinical association of LV function parameters and mortality already exists. Our task is to estimate a preliminary accurate associations of these parameters to mortality with candidate co-variates in mind. Demographic, laboratory, clinical, and other TTE findings are potential co-variates. The most clinically-relevant of these include age, sex, BMI, number of co-morbidities, Troponin I, presence of severe complications and COVID-19 severity.
Log-rank Tests
A Log-rank test was performed to examine the relation between GLS and in-hospital mortality. GLS and in-hospital mortality had a χ2 (1, N =123) = .443, p = .506. Mean and median survival times were created (Table 7).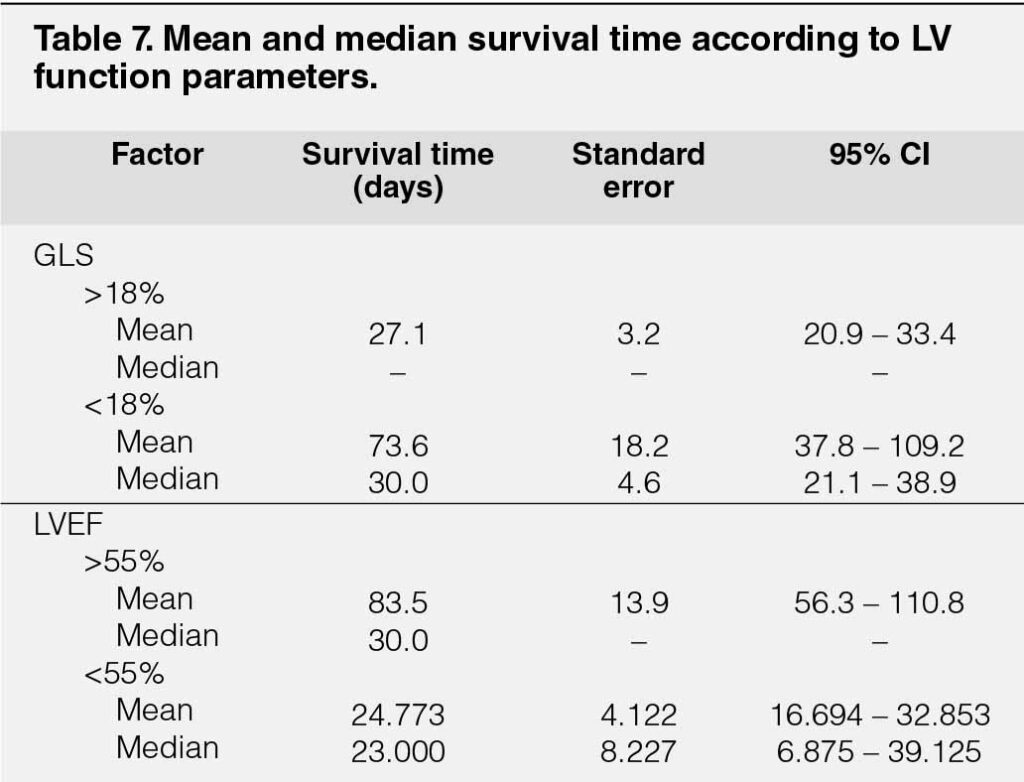
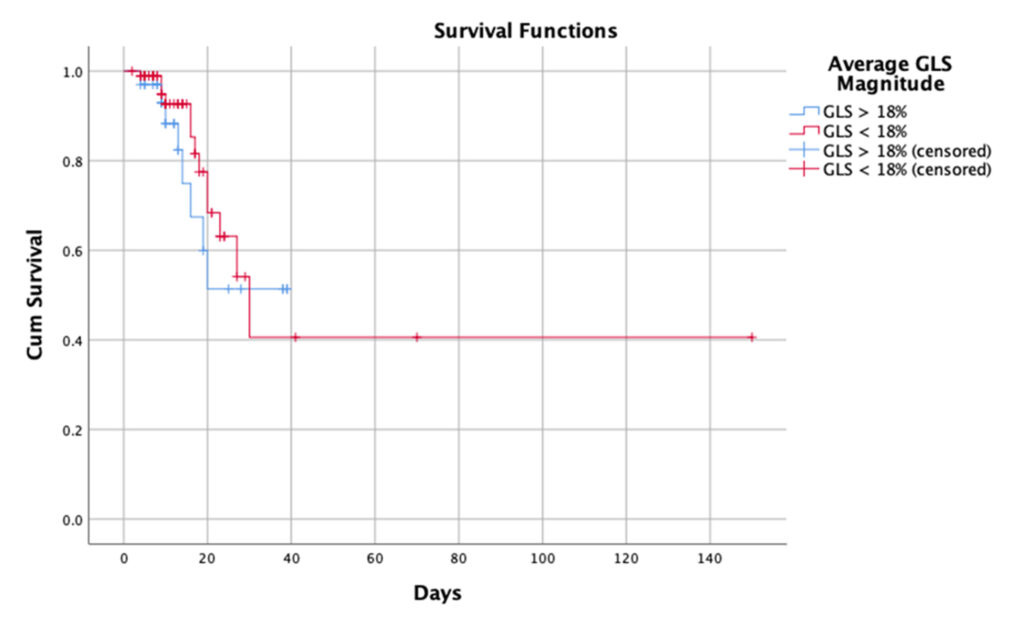
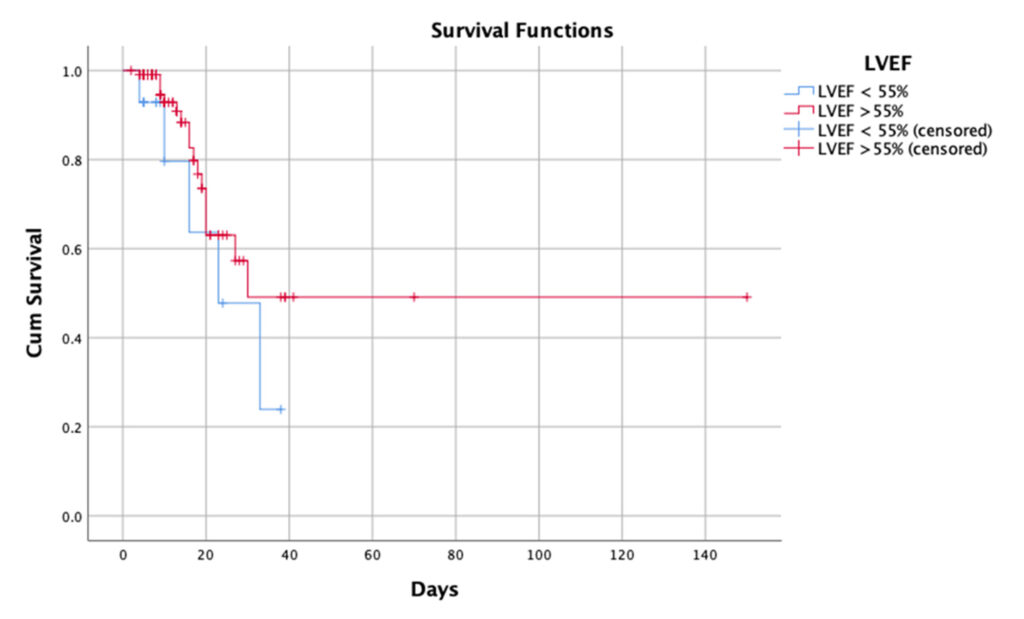
On inspection, it is seen that the survival curves of GLS and LVEF crossed; (Figure 2) the log-rank test may be unreliable due to an increased risk for a type II error and the lower power of the test. The authors understand that a multivariable model may perform a better determination of association and showcase confounders.
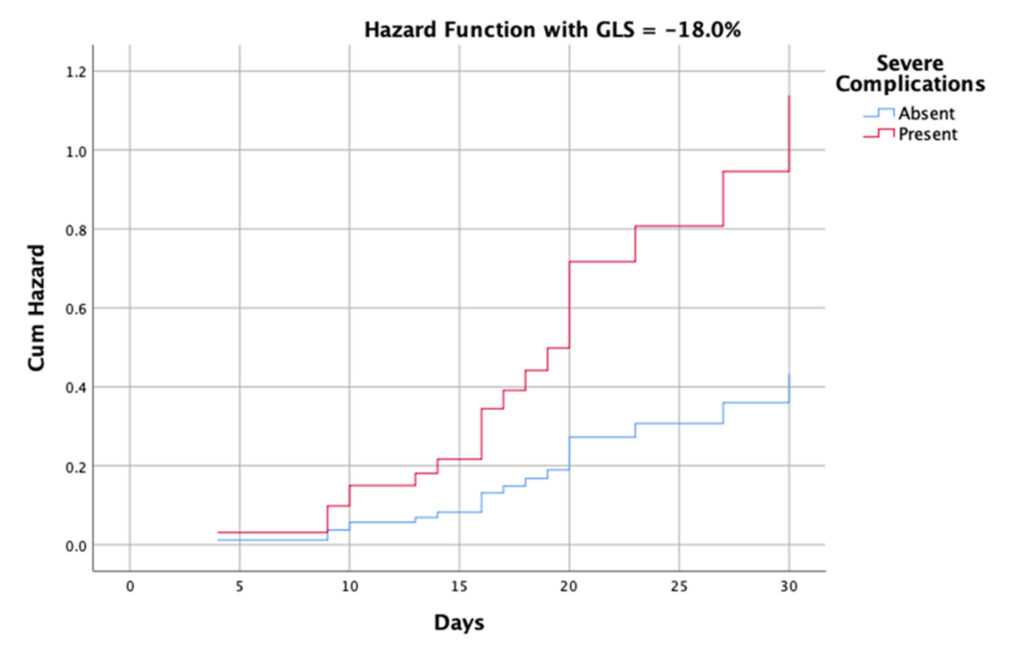
Cox PH regression
All potential continuous and categorical variables passed all the assumptions of Cox PH regression (p > .050). A model was created using GLS as a main factor with pre-selected co-variates with a Wald χ2 (2, N = 121) = 7.932 (p = .020). (Table 8) Co-variates were average GLS magnitude (HR = 0.897 [95% CI 0.808 to 0.997], p = .0.043) and presence of severe complications (HR = 2.630 [95% CI of 1.087 to 6.362], p = 0.032). Hazard functions were plotted at GLS = 18.0% and based on the presence or absence of severe complications. (Figures 4 and 5)
DISCUSSION
Although the sample size may not have reached the desired number, previous studies have had samples ranging from 31 to 214.17 This number is partially limited by the number of COVID patients admitted during the timeframe during which this study was carried out. This study was done during the tail-end of the second large surge of infections in the Philippines thus explaining the larger number of patients during the first month and a sudden drop off during the second month. They were admitted at a mean of 8 days from first symptoms and majority of them were eventually diagnosed as at least severe and even critical with only 25 moderate cases admitted and one mild case in the population. Of note is the diagnosis of myocarditis being made in only three patients, of which, only one had proven evidence of decreased left ventricular ejection fraction by a repeat 2D echocardiogram. This may be attributed to the lack of specific criteria of diagnosis and inconsistent reporting as noted by Siripanthong et al who reviewed claims that up to 7% of COVID-19 deaths may be due to myocarditis.23 Troponin I levels were elevated in 68.6% of patients in who it was requested but were not used as basis for the diagnosis of myocarditis as the diagnosis was only made in three patients.
The transthoracic 2D Echos performed were often done on admission or within one day of admission and may be representative of the patient’s status on admission. Left ventricular ejection fraction was found to be normal in most of these patients as well and were found to have normal wall motion and contractility. Global longitudinal strain on the other hand was found to have a normal mean with a value below -18% but 73.2% of patients were noted to have an average global longitudinal strain of greater than the reference value of -18%, indicating decreased and abnormal global longitudinal strain in the population.
The decreased average global longitudinal strain however was only found to have a significant association with Troponin I, and not with D-dimer or proBNP, all three of which have been found to have an association with mortality.20 A decreased ejection fraction demonstrated a similar association with an elevated Troponin I and lack thereof with proBNP and D-dimer.
As stated, the vast majority of patients in the study had left ventricular ejection fractions that fell into the normal range. With this in mind, it is understandable that the Kaplan-Meier log-rank showed no significant association between an abnormal left ventricular ejection fraction and in hospital mortality (Figure 3). It was also noted patients in this population were found to have an abnormal average global longitudinal strain in the majority of cases and the Kaplan-Meier log-rank also showed no significant association between average global longitudinal strain and in-hospital mortality. This population distribution may have skewed the results leading to the non-significance of findings. Review of the curves suggest the presence of confounding variables. This led to the development of a multivariate model to analyze the effect of other variables as was seen in similar studies.14, 21, 22 A decreased left ventricular ejection fraction was then found significant in a model that included severe complications, advanced age in years, and critical covid as significant covariants but including male sex, and average global longitudinal strain. Average global longitudinal strain was not found to be significant in this model .This demonstrated the confounding effects of these variables. The development of the model with average global longitudinal strain magnitude as the main factor was then done. The multivariate analysis found that a higher average global longitudinal was associated with improved survival with a significant hazard ratio of 0.897 when controlled for the presence of severe complications. This is suggestive of the significance of average global longitudinal strain in predicting the chances of avoiding in-hospital death.
Similar studies are in agreement with findings of abnormal and decreased average global longitudinal strain among patients with COVID-19, however the mean average global longitudinal strain was found to be much higher than those previously observed. This may be explained by the timing of 2D Echos done in previous studies which were much later, usually in the latter half of admission. 3, 12, 22 This is in contrast to the timing in this study where a large number of the studies were done within a day of admission.
The association of Troponin I with cardiac injury and the association increased levels with increased mortality has been established by previous studies along with levels of proBNP and D-dimer.24 Li et al found significant association between Troponin I and proBNP which continued to be significant after adjusting for age and sex.3 This supports with the findings in our study where an abnormal Troponin I was associated with an abnormal average global longitudinal strain. However, an association between average global longitudinal strain and proBNP was not found. This could be explained by the inconsistent request for proBNP in the population. The association between Troponin I and average GLS could be explained by myocardial injury occurring in COVID-19 also having an effect on myocardial contractility and function as detected by average global longitudinal strain.15 Baycan et al found similar results associating Troponin I levels with disruption of left ventricular longitudinal strain which they claim as proof of myocardial damage.21 They also found a significant relationship between the left ventricular Global longitudinal strain value and D-dimer that was not seen in this study. This association with Troponin I, points towards the utility of global longitudinal strain in COVID-19.
A majority of the patients enrolled in the study showed average GLS values below the lower limit of normal suggesting that patients with COVID-19 infection may have lower GLS. The significance of the association found in this study between GLS and mortality may be interpreted that the degree of myocardial contractility on admission as measured by GLS was found to be predictive of mortality after controlling for the presence of severe complications. The development of a preliminary model showed the ability to predict mortality based on measured GLS on admission and the occurrence or presence of severe complications during admission, which was also found to be of significance in the model produced. A higher GLS was thus found to be associated with decreased chances of mortality and thus increased survival but could be affected along the course of the admission by the development of additional complications. This model was different from those of previous studies but was found to have significance in this study. Although previous studies were designed to measure the effect of COVID-19 on GLS by with TTE’s done later during the admission, similar results were attained with a significant association between GLS level and mortality.3, 12, 22 Baycan et al controlled for the most variables by excluding patients with segmental wall motion, and other factors that may decrease GLS, did the TTE’s with a similar timeframe to this study and found that GLS was still associated with increased levels of D-dimer and Troponin I which detected myocardial injury associated with the severity of the disease and mortality.21 Hypertension was also prevalent in this population and is notable because a study by Croft et al found a similar prevalence in their study which did not find a significance to prediction of hospital death or mechanical ventilation, but did report a trend towards its predication.10 A similar study by Kim et al found a greater prevalence of hypertension in the more severe group but found no significant difference in GLS between the two groups.12 The prevalence of hypertension in the study is of note due to its effect of decreased GLS in patients with this comorbidity. A model produced by Lassen et al included hypertension, DM, BMI, smoking status, sex and age and also showed a higher risk of dying with reduced GLS.14 Li et al set a higher cutoff of 21% as compared to the 18% used in this study and was also taken at a time past the critical period of the disease, confirmed that GLS was associated with markers of more severe disease, including Troponin I and proBNP, as well as inflammatory cytokines (IL6, TNF) and Sp02 levels and thus concluded the prevalence of myocardial dysfunction. This highlights the potential pathophysiology behind COVID-19 induced cardiac dysfunction.3
Generalized inflammation causing disruption of plaques was also postulated by Lassen et al.14 None of the studies could confirm with certainty that direct cardiac injury was due to COVID-19 infection due to lack of baseline and follow up studies of GLS. Lassen et al admitted that myocardial insufficiency may have been present prior to the study and they were unable to control for it.14 The effect of the occurrence of severe complications on the survival and hazard curve can thus be explained by mortality being predicted by cardiovascular function and reserve and being further strained by the occurrence of one or more complications thus leading to systemic collapse and a patient’s demise. Liu et al found increased left ventricular mass and pericardial effusion in COVID-19 patients postulating that it could be indicative of a heart swelling. A small number of autopsies done in this study showed myocardial edema, inflammatory cells and enlargement of myocytes. They hypothesized that such swelling may be caused by fluid overloading or the cytokine storm of COVID-19. Such edema can also explain the abnormal GLS in these patients.14
CONCLUSIONS
The study was able to develop a preliminary model for predicting mortality based on GLS and adjusting rates based on the occurrence of severe complications during admission. This model may be useful in practice to explain to patients the predicted course and the effects of any complications allowing one to stress the importance of interventions to protect against such complication. We can therefore conclude from this study that among patients admitted for COVID-19 an abnormal average global longitudinal strain predicts increased mortality.
Limitations
The study is primarily limited by its sample size which fell well short of the computed sample size of 167. Despite this, a significance was still found in the study which may be strengthened by a larger sample size. Selection bias limited the patients to those who had images where average global longitudinal strain studies could be done. The descriptive data was taken from a this specific sample of patients who had transthoracic echocardiograms done during their admission based on clinician judgement which may inadvertently have led to milder and less complicated cases being excluded. Laboratories were also requested based on physician judgement and could not be controlled. As stated earlier, the distribution of global longitudinal strain and left ventricular ejection fraction may also lead to some bias in the computation of statistics that was minimized through multivariate analysis. Due to the study design, we cannot make conclusions on the causality between COVID-19 and the decreased average global longitudinal strain. Further prospective study with a larger sample size may be able to achieve a model with increased precision, accuracy and reliability.KEY WORDS
COVID-19, 2D echocardiogram, Transthoracic echocardiography, left ventricular global longitudinal strain, in-hospital mortality
ACKNOWLEDGMENTS
We would like to acknowledge the efforts of Erickson Torio, MD in assisting in the design and statistical analysis of the study, as well as Renato Ong, MD for his invaluable input in the writing of the final paper for publication.
REFERENCES
1. Updates of Novel Coronavirus Disease (COVID-19). 2021 May 20, 2021 [cited 2021 May 21, 2021]; Available from: https://doh.gov.ph/2019-nCoV.
2. Bryce, C., et al., Pathophysiology of SARS-CoV-2: the Mount Sinai COVID-19 autopsy experience. Mod Pathol, 2021. CrossRef Pubmed
3. Li, R., et al., Widespread myocardial dysfunction in COVID-19 patients detected by myocardial strain imaging using 2-D speckle-tracking echocardiography. Acta Pharmacol Sin, 2021. CrossRef Pubmed
4. Gackowski, A., et al., Echocardiography during the coronavirus disease 2019 (COVID-19) pandemic: expert opinion of the Working Group on Echocardiography of the Polish Cardiac Society. Kardiol Pol, 2020. 78(4): p. 357-363. CrossRef Pubmed
5. Hung, J., et al., ASE Statement on the Reintroduction of Echocardiographic Services during the COVID-19 Pandemic. J Am Soc Echocardiogr, 2020. 33(8): p. 1034-1039. CrossRef Pubmed
6. Ward, R.P., et al., Utilization and Appropriateness of Transthoracic Echocardiography in Response to the COVID-19 Pandemic. J Am Soc Echocardiogr, 2020. 33(6): p. 690-691. CrossRef Pubmed
7. Voigt, J.U., et al., Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging, 2015. 16(1): p. 1-11. CrossRef Pubmed
8. Lang, R.M., et al., Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr, 2015. 28(1): p. 1-39 e14. CrossRef Pubmed
9. Zeng, J.H., et al., Cardiac manifestations of COVID-19 in Shenzhen, China. Infection, 2020. 48(6): p. 861-870. CrossRef Pubmed
10. Croft, L.B., et al., Abnormal left ventricular global longitudinal strain by speckle tracking echocardiography in COVID-19 patients. Future Cardiol, 2020. CrossRef Pubmed
11. Solomon, M.D., et al., The Covid-19 Pandemic and the Incidence of Acute Myocardial Infarction. N Engl J Med, 2020. 383(7): p. 691-693. CrossRef Pubmed
12. Kim, M., et al., Cardiac Manifestations of Coronavirus Disease 2019 (COVID-19): a Multicenter Cohort Study. J Korean Med Sci, 2020. 35(40): p. e366. CrossRef Pubmed
13. Lairez, O., et al., Cardiac imaging phenotype in patients with coronavirus disease 2019 (COVID-19): results of the cocarde study. Int J Cardiovasc Imaging, 2021. 37(2): p. 449-457. CrossRef Pubmed
14. Lassen, M.C.H., et al., Echocardiographic abnormalities and predictors of mortality in hospitalized COVID-19 patients: the ECHOVID-19 study. ESC Heart Fail, 2020. CrossRef Pubmed
15. Liu, Y., et al., Swollen heart in COVID-19 patients who progress to critical illness: a perspective from echo-cardiologists. ESC Heart Fail, 2020. CossRef Pbmed
16. Vera-Pineda, R., et al., Echocardiographic Characteristics of Subjects With COVID-19: A Case Series. Cardiol Res, 2020. 11(4): p. 260-265. CrossRef Pubmed
17. Wibowo, A., et al., Left and right ventricular longitudinal strains are associated with poor outcome in COVID-19: a systematic review and meta-analysis. J Intensive Care, 2021. 9(1): p. 9. CrossRef Pubmed
18. Zou, Fengwei et al. “Cardiac Injury and COVID-19: A Systematic Review and Meta-analysis.” CJC open vol. 2,5 (2020): 386-394. doi:10.1016/j.cjco.2020.06.010 CrossRef Pubmed
19. Lyngbakken, M.N., et al., Cardiac Troponin I and T Are Associated with Left Ventricular Function and Structure: Data from the Akershus Cardiac Examination 1950 Study. Clin Chem, 2020. 66(4): p. 567-578. CrossRef Pubmed
20. Balaban Kocas, B., et al., The relation between left ventricular global longitudinal strain and troponin levels in patients hospitalized with COVID-19 pneumonia. Int J Cardiovasc Imaging, 2021. 37(1): p. 125-133. CrossRef Pubmed
21. Baycan, O.F., et al., Evaluation of biventricular function in patients with COVID-19 using speckle tracking echocardiography. Int J Cardiovasc Imaging, 2021. 37(1): p. 135-144. CrossRef Pubmed
22. Janus, S., Hajjari, J., Karnib, M. , Tashtish, N., Al-Kindi, S., Hoit, B., Prognostic Value of Left Ventricular Global longitudinal strain in COVID-19. The American Journal of Cardiology, 2020. 131: p. 134-136. CrossRef Pubmed
23. Siripanthong, Bhurint et al. “Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management.” Heart rhythm vol. 17,9 (2020): 1463-1471. doi:10.1016/j.hrthm.2020.05.001 CrossRef Pubmed
24. Sheth, Aakash et al. “Prognostic value of cardiac biomarkers in COVID-19 infection.” Scientific reports vol. 11,1 4930. 2 Mar. 2021, doi:10.1038/s41598-021-84643-6 CrossRef Pubmed
25. Oikonomou, Evangelos K et al. “Assessment of Prognostic Value of Left Ventricular Global Longitudinal Strain for Early Prediction of Chemotherapy-Induced Cardiotoxicity: A Systematic Review and Meta-analysis.” JAMA cardiology vol. 4,10 (2019): 1007-1018. doi:10.1001/jamacardio.2019.2952 CrossRef Pubmed
26. Hu, Jianhua, and Yanggan Wang. “The Clinical Characteristics and Risk Factors of Severe COVID-19.” Gerontology vol. 67,3 (2021): 255-266. doi:10.1159/000513400 CrossRef Pubmed
27. Kollias, Anastasios et al. “Venous thromboembolism in COVID-19: A systematic review and meta-analysis.” Vascular medicine (London, England) vol. 26,4 (2021): 415-425. doi:10.1177/1358863X21995566 CrossRef Pubmed
Copyright Information
