Case Report
July 2023, 32:2
First online: 9 July 2023
Case Report
Successful Minimally Invasive Mitral Valve Replacement in a Post-thymectomy Patient with Myasthenia Gravis: A Case Report
Joseph Lawrence Ponciano, MD,1 Jeannica Kriselle Lerios-Dela Pena, MD 1
Main author’s email: joloponciano@gmail.com
ABSTRACT
Presented is a case of a 68-year-old Filipino, female, a known case of Myasthenia Gravis, post-thymectomy maintained on pyridostigmine, with a history of hypertension and Mitral Valve Prolapse who was admitted for acute heart failure symptoms. Diagnostics revealed a torn chordae tendineae of the mitral valve and the patient was subsequently advised to undergo mitral valve replacement due to acute decompensation. Pre operative coronary evaluation showed angiographically normal coronary arteries while CT aortogram showed no distinct evidence of aortic aneurysm, stenosis, dissection or severe calcification of thoraco-abdominal aorta and iliac-femoral vessels. The patient underwent minimally invasive mitral valve replacement with a bioprosthetic valve, however suddenly experienced ptosis and respiratory depression while at the recovery room which were attributed to stress from surgery and missed doses of Pyridostigmine while undergoing surgery. She was closely monitored at the Intensive Care Unit and her symptoms gradually resolved upon resumption of Pyridostigmine. Despite the unanticipated respiratory depression and ptosis, the patient was able to complete 5 days of phase I cardiac rehabilitation post operatively and was discharged well and improved. The case reported may be the first locally documented ruptured chordae tendineae with coinciding Myasthenia Gravis who underwent minimally invasive valve replacement with successful treatment outcomes.INTRODUCTION
Myasthenia Gravis (MG) is an autoimmune disorder which affects the neuromuscular system. It is estimated to affect more than 700,000 people with incidence from 0.3-2.8 per 100,000 worldwide.1 It results from decreased number of active acetylcholinesterase receptors at the neuromuscular junction by either destruction or functional block of the receptors by circulating antibodies.2 Signs and symptoms include diplopia, body weakness and dyspnea with severity of the disease dependent on the group of muscles involved. It follows a slow progressive course that becomes generalized and may become fatal when respiratory muscles fail.1 On the other hand, ruptured chordae tendineae is a common cause of mitral valve incompetence leading to acute mitral valve regurgitation.3 The combination of MG and mitral valve disease is a rare occurrence which may preclude a catastrophe, especially during cardiac surgery as definitive treatment for ruptured chordae tendinae.4 The decision to proceed with cardiac surgery among these patients is a serious medical dilemma since life-threatening complications are often encountered among post-thymectomy patients with Myasthenia Gravis. This paper presents a rare case of ruptured chordae tendinea with flail leaflet in a post thymectomy patient diagnosed of MG who underwent successful minimally invasive cardiac surgery.
CASE
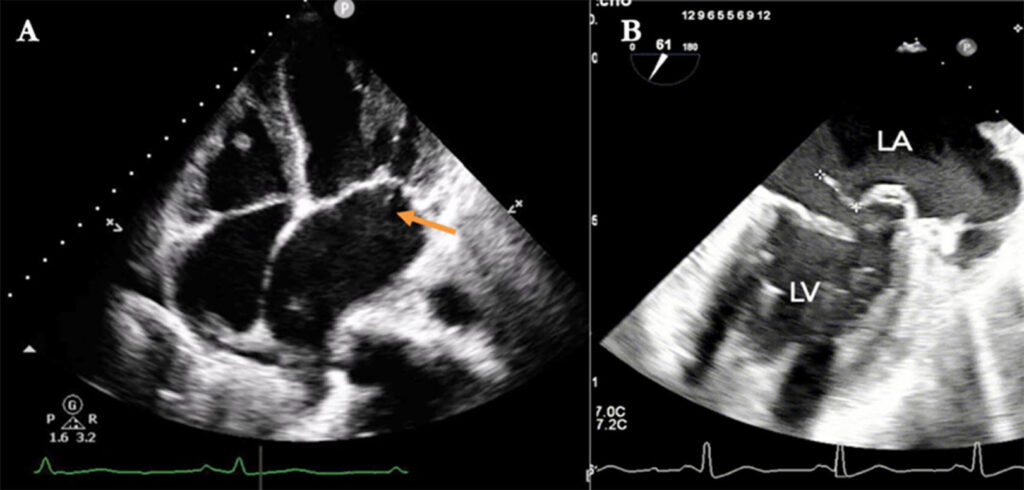
Presented is a 68-year-old Filipino, female admitted for heart failure symptoms. Past medical history was pertinent for hypertension, Mitral Valve Prolapse and MG, post-thymectomy ten years prior via midline sternotomy and was maintained on Pyridostigmine. One month prior to admission, after routine follow up, patient’s 12-lead electrocardiogram revealed sinus rhythm with ischemic changes while coronary CT scan showed dilated left ventricle with normal systolic function, dilated left atrium with consideration of ruptured chordae of posterior mitral valve, however was lost to follow-up thereafter. Patient had a three weeks history of progressive exertional dyspnea, two-pillow orthopnea and paroxysmal nocturnal dyspnea which prompted consultation.At the emergency room, patient was in distress with initial vital signs of BP 100/60mmHg, HR 80bpm, RR 34cpm, afebrile, 80% at room air. Physical examination revealed distended neck veins, bibasal crackles, regular cardiac rhythm with holosystolic murmur at the apex 3-4/6 severity, no S3 or S4 gallop with grade 2 pitting bipedal edema. No improvement was noted with 15 LPM oxygen support hence, patient was hooked to Bilevel Positive Airway Pressure (BPAP). 12-lead electrocardiogram showed regular sinus rhythm with left atrial and left entricular hypertrophy, NT pro-BNP was 748 pg/ml (< 125 pg/ml), chest Xray showed bilateral pleural effusion, bilateral pneumonia with pulmonary congestion, COVID-19 RT PCR revealed negative. The patient was managed as decompensated heart failure secondary to possible torn chordae tendineae and was started with diuretics and nitrates for heart failure and broad-spectrum antibiotics for pneumonia. Neurology referral was facilitated and continued Pyridostigmine at 60mg/tab, 1 tab thrice daily. During admission, transthoracic 2D-echocardiogram showed anterior mitral valve prolapse with flail with severe mitral regurgitation, dilated left ventricle with normal systolic function, left ventricular end systolic diameter of 35mm, biatrial dilatation and systolic pulmonary artery pressure of 43mmHg. Transesophageal echocardiogram further revealed prolapsed A1, P1 and anterolateral commissure with flail P1 scallop and an echogenic density attached to posterior leaflet likely a torn cord (Figure 1). Plan of management was minimally invasive mitral valve replacement and the patient was counselled well on the course of surgery and possible complications that may be encountered due to preexisting medical conditions.
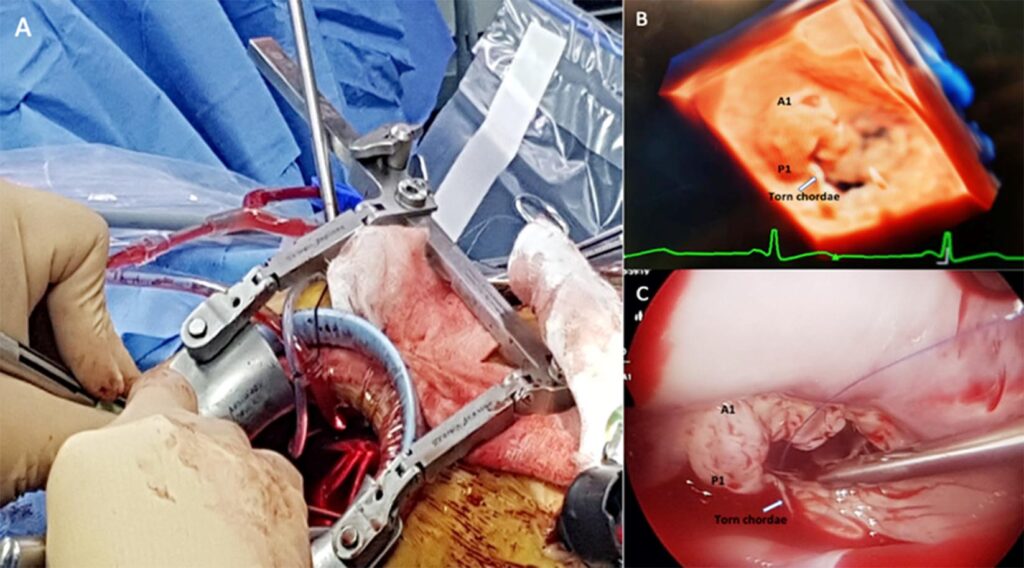
The patient received Pyridostigmine on the morning of surgery. General anesthesia was induced with Sevoflurane, Propofol and Fentanyl. A right mini-thoracotomy incision was made to access the mitral valve thru the right anterior axillary 4th intercostal space (Figure 2A). A bioprosthetic valve (St. Jude Medical Epic Valve size 27 mm) was implanted. Immediate post-operative transesophageal echocardiogram showed normal functioning bioprosthetic mitral valve with no paravalvular leak. Transient ptosis and increased work of breathing were observed postoperatively. From Neurology standpoint, at this time, the probable cause of symptoms was mainly attributed to missed doses of Pyridostigmine during surgery and from the stress that entailed her surgery. Monitoring and close observation were continued at the intensive care unit (ICU). Patient’s symptoms gradually resolved with the resumption of Pyridostigmine. Patient tolerated mechanical ventilation weaning and was successfully extubated. After 4 days of close monitoring in the ICU, the patient was then transferred to telemetry ward and completed Phase I cardiac rehabilitation and was discharged well with the following home medications: Warfarin at 2.5 mg/tab 1-tablet once daily, Irbesartan 150 mg tab, 1-tablet once daily, Diltiazem 90 mg/tab, 1-tablet once daily, Pyridostigmine 60mg/tab 1-tablet thrice daily.
DISCUSSION
The presented case was a rare combination of torn mitral chordae tendineae with flail leaflet in an MG patient presenting with acute heart failure symptoms. It has been a standard of care for symptomatic patients with severe mitral regurgitation to undergo surgical treatment.5 However, there are few reports on how patients with MG undergoing cardiac surgery should be managed. In general, muscle relaxants are used during cardiac surgery however, this may impair the cardiorespiratory system of MG patients. Unnecessary prolonged postoperative mechanical ventilation may predispose cardiac surgical patients to undesired complications.6, 7 Different anesthetic techniques are recommended among MG patients but none of them is proven to be superior over the other. Guerent et al8 reported that muscle relaxants are not necessary in patients undergoing cardiac surgery which may be beneficial in patients with Myasthenia Gravis. Development of MG after open heart surgery and recurrences may be observed among thymectomized patients. It was suggested that MG recurrence or exacerbation after cardiac surgery even without muscle relaxants may be due to the damage on the thymic remnants during mediastinal exploration which causes release of the myoid cells that express whole AChR molecules.9 This finding could contribute to the etiology of recurrence or exacerbation in Myasthenia Gravis patients on remission after sternotomy.10
At the time of writing, all reported cases of mitral valve surgery in MG patients underwent conventional open-heart surgery. Minimally invasive cardiac valve surgery is a new and evolving surgical approach which utilizes small right mini thoracotomy incision for mitral valve replacement. The study of Zhai et al11 proved the safety and efficacy of minimally invasive mitral valve replacement consistent with the results of conventional open cardiac surgery, with the advantages of a small incision, minimal trauma, and quick recovery. This case may be the first reported case of myasthenia Gravis who underwent minimally invasive mitral valve replacement, with successful treatment outcomes.
Minimally invasive cardiac valve surgery may be successfully performed among MG patients through timely diagnosis, careful heart team planning, multidisciplinary care and appropriate anesthetic agents, which were all employed in this patient.
Keywords
Myasthenia Gravis, pyridostigmine, ruptured chordae tendineae, minimally invasive mitral valve surgery
ACKNOWLEDGEMENT
The authors would like to acknowledge all attending physicians involved in the management of the case, your invaluable contribution has made this case a success. Special thanks to our beloved The Medical City Cardiology Department and our cardiology consultants for their unwavering support and provision of inspiration, nothing else but much gratitude.REFERENCES
1. Deenen JC, Horlings CG, Verschuuren JJ, Verbeek AL, van Engelen BG. The epidemiology of neuromuscular disorders: a comprehensive overview of the literature. J Neuromuscul Dis 2015;2(1):73-85. Pubmed
2. Vincent A, Palace J, Hilton-Jones D. Myasthenia gravis. Lancet
2001;357:2122-2128. CrossRef Pubmed
3. Gabbay U, Yosefy C. The underlying causes of chordae tendinae rupture: A systematic review. Int J Cardiol. 2010 Aug 20;143(2). CrossRef Pubmed
4. Dubost C, Carpentier A, Piwnica A, et al. A surgical series of 128 cases of mitral insufficiency caused by chordae tendineae rupture. Arch Mal Coeur Vaiss 1975;68: 29-34. Pubmed
5. 2021 ESC/EACTS Guidelines for the Management of Valvular Heart Disease. European Heart Journal (2022) 43, 561-632. CrossRef Pubmed
6. Buzello W, Pollmaecher T, Schluermann D, et al: The influence of hypothermic cardiopulmonary by- pass on neuromuscular transmission in the absence of muscle relaxants. Anesthesiology 1986;64:279-281. CrossRef Pubmed
7. Buzello W, Schluermann D, Schindler M, et al: Hypothermic cardiopulmonary bypass and neuromuscular blockade by pancuronium and vecuronium. Anesthesiology 1985;62:201-204. CrossRef Pubmed
8. Guerent G, Rossignol B, Kiss G, et al: Is muscle relaxant necessary for cardiac surgery? Anesth Analg 2004;99:1330-1333. CrossRef Pubmed
9. Scoppetta C, Onorati P, Eusebi F, et al: Autoimmune myasthenia gravis after cardiac surgery. J Neurol Neurosurg Psychiatry 2003;74:392-393. CrossRef Pubmed
10. Narin et al: Successful Mitral Valve Surgery in a Patient with Myasthenia Gravis. J CARD SURG 2009;24:209-222. CrossRef Pubmed
11. Zhai et al: Minimally invasive mitral valve replacement is a safe and effective surgery for patients with rheumatic valve disease: A retrospective study. Medicine (2017) 96:24(e7193). CrossRef Pubmed
Copyright Information
