Case Report
August 2025, 34:2
First online: 18 August 2025
Case Report
Acute Upper Limb Ischemia in an Octogenarian with Chronic Atrial Fibrillation and Previous CABG: A Multidisciplinary Approach to Limb Salvage
Jamelen R. Narvasa,1 Katrina Buton-Nabong,1 Charisse Mendoza-Aldea1
Main Author’s Name: Jamelen R. Narvasa
Main Author’s Contact Details: Email Address: jamnarvasa@gmail.com
Cellular Number: +639064362218
ABSTRACT
An 86-year-old man with hypertension, dyslipidemia, multivessel coronary artery disease post coronary artery bypass graft (CABG), and chronic atrial fibrillation (AF) presented with acute numbness, weakness, and discomfort in his left arm. The left ulnar artery exhibited diminished blood flow during the examination. Ultrasound imaging showed an acute thrombus, and anticoagulation with heparin was initiated. A thrombectomy was performed, successfully removing the thrombus. Postoperative evaluation confirmed restored blood flow with no residual thrombus. The patient was discharged on warfarin. This case highlights the management of acute limb ischemia in atrial fibrillation and the importance of anticoagulation in preventing thromboembolic events.
Keywords
Acute limb ischemia, Atrial Fibrillation, Thromboembolism
INTRODUCTION
Acute limb ischemia constitutes a critical vascular emergency necessitating immediate identification and action. In patients with atrial fibrillation or those who have undergone coronary artery bypass graft with radial artery harvesting, understanding the relationship between these disease entities is necessary to achieve better outcomes. Timely surgical consultation and intervention can significantly enhance outcomes and maintain limb function.
CASE PRESENTATION
This is a case of an 86-year-old man with hypertension, dyslipidemia, and multivessel coronary artery disease who underwent CABG in 2005. The patient also had chronic atrial fibrillation that began in 2018 and was previously on an unrecalled oral anticoagulant that was only used for a few months before discontinuing; patient was then lost to follow up with his cardiologist. The patient appeared to be in good health until a few hours prior to consult, there was a sudden onset of numbness in the patient’s left arm, accompanied by weakness in hand grip and an aching pain. The patient was noted to have an elevated systolic blood pressure of 200 mmHg systolic while at home. No interventions were taken at that time. The patient reported no chest pain, headache, or dizziness. After an hour, blood pressure was rechecked, which had decreased slightly to 190 mmHg systolic. As the symptoms persisted, a physician was consulted who prescribed one tablet of clonidine, providing partial relief. After a few hours, due to persistent symptoms, the patient sought second opinion and was advised to return to the hospital, where the patient was subsequently admitted.
Upon examination, the patient exhibited stable vital signs; however, the left upper extremity was poikilothermic and pale from the forearm to the hand. The left upper extremity had 2+ brachial pulse, with an absent Doppler signal on the ulnar artery whereas the right upper extremity showed normal findings.
Cardiology service initiated Enoxaparin 60mg subcutaneously twice daily and administered paracetamol 600 mg intravenously every 6 hours as needed for pain relief. A stat duplex ultrasound of the arterial and venous systems was performed which revealed acute to subacute thrombus formation in the proximal ulnar artery, resulting in attenuated downstream flow, a surgically absent radial artery and no demonstrable venous thrombosis (Figure 1A). The CBC, troponin I, HS, D-dimer, electrolytes and creatinine were unremarkable whereas 12L ECG taken showed findings of AF and a prolonged QT interval. Patient was admitted as a case of acute limb ischemia of the left ulnar artery, Rutherford IIB likely cardioembolic and chronic atrial fibrillation. The patient was additionally referred to the Vascular Medicine service. Enoxaparin was shifted to Heparin infusion which was started at 18 units per kilogram per hour. Vascular Surgery service was consulted for endovascular management. The patient then underwent ulnar angiography with thrombectomy and intraoperative findings include evacuated clots distal from brachial artery using Fogarty French three, with no subsequent filling defects/cut noted on angiogram (Figure 2).
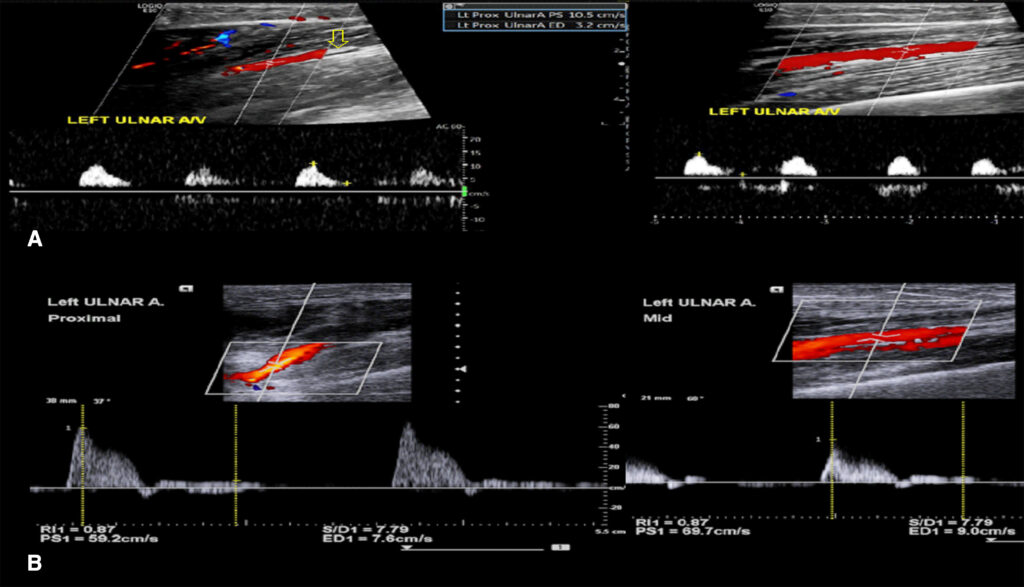
Panel A (Pre-thrombectomy): Medium level echoes seen almost completely filling the lumen of the proximal ulnar artery, consistent with thrombus formation (yellow arrow), with downstream attenuation of flow and tardus parvus waveforms—consistent with significant arterial obstruction. No collateral vessel formation seen.
Panel B (Post-thrombectomy): The previously noted thrombus in the left ulnar nerve is no longer observed. Restoration of triphasic flow patterns is noted in all segments of the ulnar artery, with significantly increased peak systolic velocities and normalized resistive indices, confirming successful thrombectomy and reperfusion.
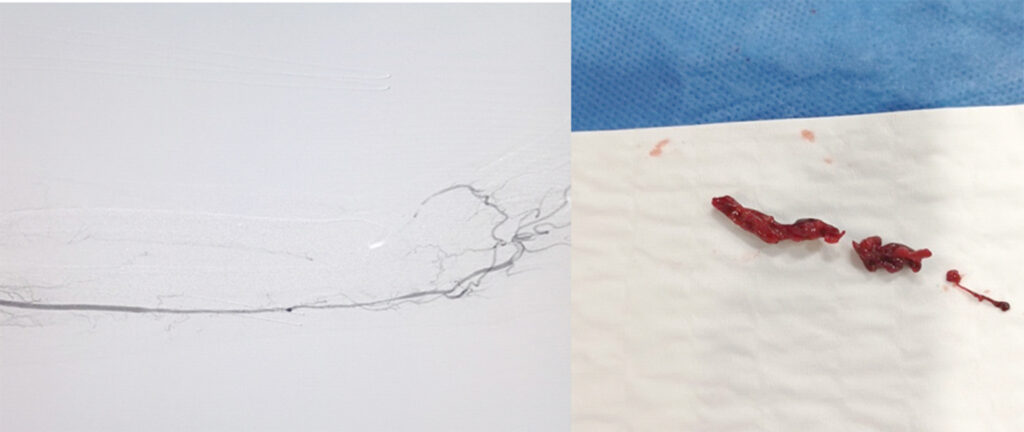
Patient postoperatively was seen awake, no pain on left hand and with stable vital signs. Dressing was dry and intact in the left antecubital fossa. On examination, noted minimal bruising; a 2+ ulnar pulse is palpable in the left hand and confirmed via handheld Doppler. Enoxaparin at 40mg subcutaneously twice daily was started. A repeat arterial Duplex scan of the left arm was then requested which revealed no evidence of hemodynamically significant stenosis in all arterial segments of left upper extremity, all arterial segments of left upper extremity have no gross plaques or thrombus with multiphasic waveform pattern and no significant increase in peak systolic velocity (PSV) (Figure 1B). The previously noted thrombus in the left ulnar artery is no longer observed. Warfarin and enoxaparin bridging was then started until such a time patient was discharged with warfarin 5mg/tab 1 tab once a day with PT/INR monitoring outpatient.
DISCUSSION
Acute limb ischemia (ALI) is characterized by a rapid, limb-threatening reduction in arterial perfusion lasting fewer than 14 days. It may arise from iatrogenic factors, embolic occlusion, or in situ arterial thrombosis.1 ALI affecting the ulnar artery is an uncommon yet critical medical illness marked by a rapid decrease in blood circulation to the hand, which may result in tissue necrosis if not urgently treated. Although there are several possible causes of ALI, thromboembolism is the most common, particularly from atrial fibrillation (AF). Patients with AF exhibit a significantly reduced occurrence of systemic embolism in comparison to strokes. Research demonstrates that although the stroke risk in AF patients is well recognized, systemic embolic events (SEEs) occur less frequently yet remain significant. SEEs occur at a frequency of approximately 0.24 per 100 patient-years, representing merely 11.5% of all thromboembolic occurrences. Merely 10% of SEES pertain to the upper extremity.2 Less than 3% of cases linked to hand ischemia are caused by ulnar artery thrombosis (UAT), a rare cause of acute limb ischemia.3
At present, the preferred treatment for acute limb ischemia caused by embolism is thromboembolectomy, typically performed using the Fogarty technique. This procedure involves transverse brachial arteriotomy through an S-shaped incision in the fossa cubiti and the evacuation of thromboembolic material with a balloon catheter.4 The CHA2DS2-VA score is a crucial clinical instrument for evaluating stroke and thromboembolism risk in patients with AF and significantly influences treatment decisions, especially in instances of AF-associated ALI. Understanding the impact of this score on management choices can improve patient outcomes. A score of 2 or higher generally indicates a strong recommendation for anticoagulation to prevent stroke and systemic embolism.5 In patients presenting with ALI, immediate initiation of anticoagulation is critical for improving outcomes and reducing the likelihood of limb loss or severe complications. The recurrence rate of arterial thromboembolism is markedly reduced (9%) in individuals undergoing anticoagulant therapy compared to those not receiving it (31%).6 In order to address concerns regarding anticoagulation and optimize treatment strategies, it is essential that physicians and patients engage in ongoing education and shared decision-making.
REFERENCES
1. Creager MA, Beckman JA, Loscalzo J. Vascular Medicine: A Companion to Braunwald’s Heart Disease. 3rd ed. Philadelphia, PA: Elsevier; 2019.
2. Bekwelem W, Connolly SJ, Halperin JL, et al. Extracranial systemic embolic events in patients with nonvalvular atrial fibrillation: incidence, risk factors, and outcomes. Circulation. 2015;132(9):796-803. doi:10.1161/CIRCULATIONAHA.114.013243. CrossRef Pubmed
3. Panchal G., Hari, J.P., Roy, N. et al. A case of acute limb ischemia due to ulnar artery thrombosis: a rare surgical challenge. Indian J Surg 83 (Suppl 1), 228–231 (2021). CrossRef
4. Andersen LV, Lip GYH, Lindholt JS, Frost L. Upper limb arterial thromboembolism: a systematic review on incidence, risk factors, and prognosis, including a meta-analysis of risk-modifying drugs. J Thromb Haemost 2013; 11: 836–44. CrossRef Pubmed
5. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2024;45(33):3314-3414. doi:10.1093/eurheartj/ehae176. CrossRef Pubmed
6. Yadav AK, et al. Lower limb ischemia in atrial fibrillation: unusual presentation. JBPKIHS. 2020;3(1):129-134. CrossRef
Copyright Information
