Case Report
Dec 2022, 31:2
First online: 31 December 2022
Case Report
Myocarditis with Complete Heart Block in a Child With COVID-19 Infection
Jose Jonas Del Rosario Pediatric Cardiologist, 1 Josephine Anne N. Ng Pediatric Infectious Disease Specialist,1 Priscilla Mae C. Rosales Pediatric Resident1
Main Author: Jose Jonas Del Rosario
Contact Information: jddelrosario1@up.edu.ph
ABSTRACT
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (COVID 19), also known as COVID 19, was first detected in 2019 as a result of a cluster of pneumonia cases in China. It is known to cause respiratory illness in a majority of cases, however myocardial involvement can be seen in 7% of cases, with even a smaller number in pediatric populations.
CASE PRESENTATION
We are presented with a 14 year old male with confirmed COVID 19 infection that is followed by a fulminant myocarditis resulting in High grade AV Block and subsequent pacemaker insertion, which is the first reported case in the pediatric
population.
DISCUSSION
Cardiac injury resulting from a recent COVID 19 infection can result to a fulminant myocarditis. This can present as arrhythmia, seen in 16.7% of cases. The mainstay of treatment is still maintaining hemodynamic stability and initiating
immunomodulatory support, however, specifically in this case resulting in third-degree AV block, pacemaker insertion may also be required.
CONCLUSION
Although severe cardiac involvement in COVID 19 infection is rare, a fulminant myocarditis is possible for some patients.
KEYWORDS
COVID 19, Myocarditis, pacemaker, arrhythmia
INTRODUCTION
At the end of 2019, a cluster of pneumonia cases in Wuhan, a city in the Hubei Province of China, were thought to stem from a novel coronavirus. This virus rapidly spread and resulted in a global pandemic, with increasing numbers with each day, affecting both adult and pediatric patients alike. It is caused by Coronavirus 2 or COVID 19, also previously known as the 2019 nCov, which is known to cause mild to moderate respiratory illness in a majority of cases. Myocardial involvement with novel coronavirus has also been reported among adults, with 7% of COVID 19 related deaths being attributable to myocarditis.1 Cardiac involvement has been previously reported in a number of cases, however severe myocardial involvement in the pediatric population has not been extensively studies. Hence, we report the first case of COVID 19 infection with myocarditis resulting in a High Grade AV Block and subsequent need for pacemaker insertion
Key Words: Covid, Myocarditis, Pacemaker, Arrhythmia, Heart Block
CASE PRESENTATION
This is a case of a 14 year old male coming in for an 8 day history of fever, colds, dry cough and diarrhea that was poorly responsive to prescribed medications. A COVID RT-PCR was done on the 3rd day of illness, revealing positive results. Strict home isolation procedures were followed and the patient was monitored at home. In the interim, the patient had persistent high grade fever with progression of watery stool and new onset difficulty of breathing, thus prompting admission on the 8th day of illness.On physical examination, he had BP of 100/60mmHg, HR 118 bopm, RR 22 cpm, O2 saturation 92% at room air. Physical examination revealed respiratory distress, and harsh breath sounds on bilateral lung fields, a normal cardiac examination, with full pulses, and CRT <2 seconds.
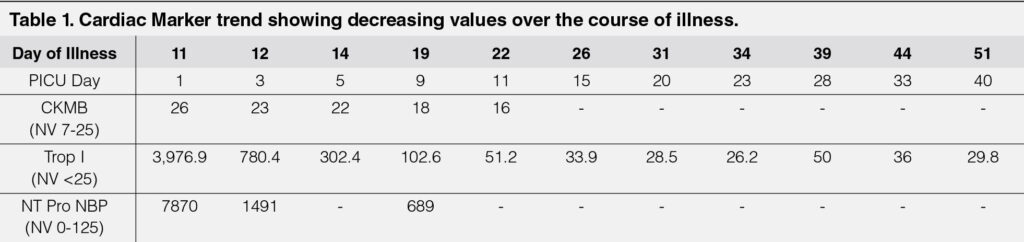
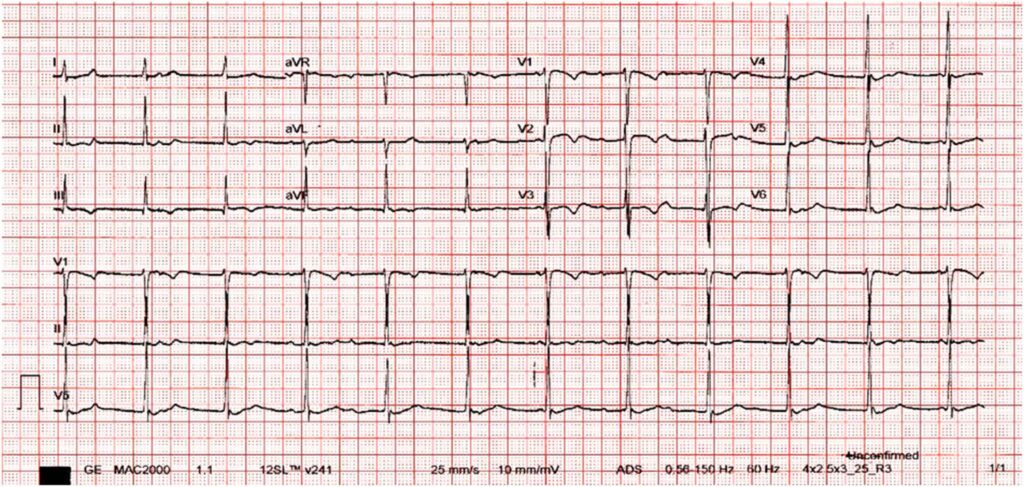
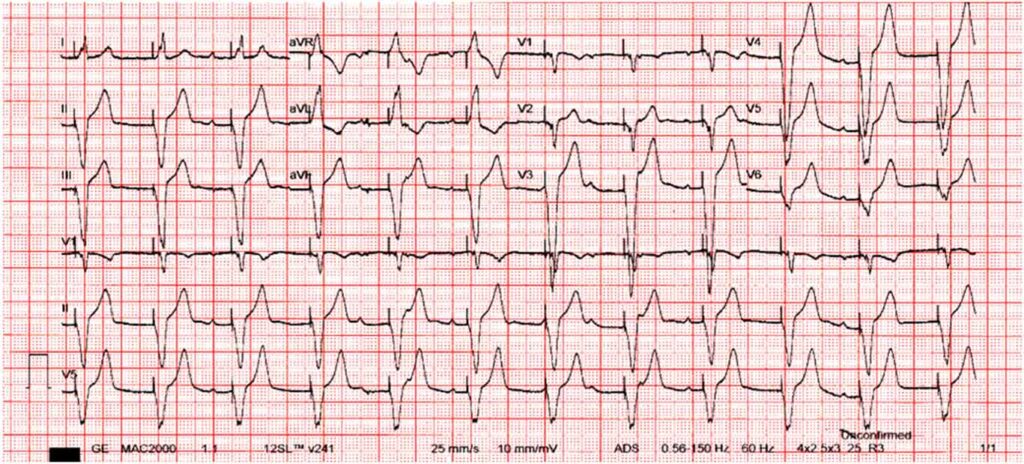
Initial workup revealed left sided pneumonia, elevated inflammatory markers, elevated cardiac markers, and an ECG showing ST-T wave changes with PR prolongation. The patient continued to have labored breathing despite O2 support, so he was later intubated and admitted into the pediatric ICU. He was treated with Remdesivir and Dexamethasone to complete 10 days, and he underwent Tocilizumab infusion on the 1st hospital day. Initial 2D Echocardiography revealed small pericardial effusion, with left ventricular systolic dysfunction and an ejection fraction of 53%. He was initially started on Milrinone, but later presented with hypotension and cardiogenic shock on the 3rd hospital day despite improving inflammatory markers (Table 1) and decreasing need for ventilatory support. The patient was, then, started on inotropic support with epinephrine on the 3rd hospital day. Further workup also revealed improving cardiac markers, but an ECG showing junctional rhythm with AV dissociation (Figure 1).
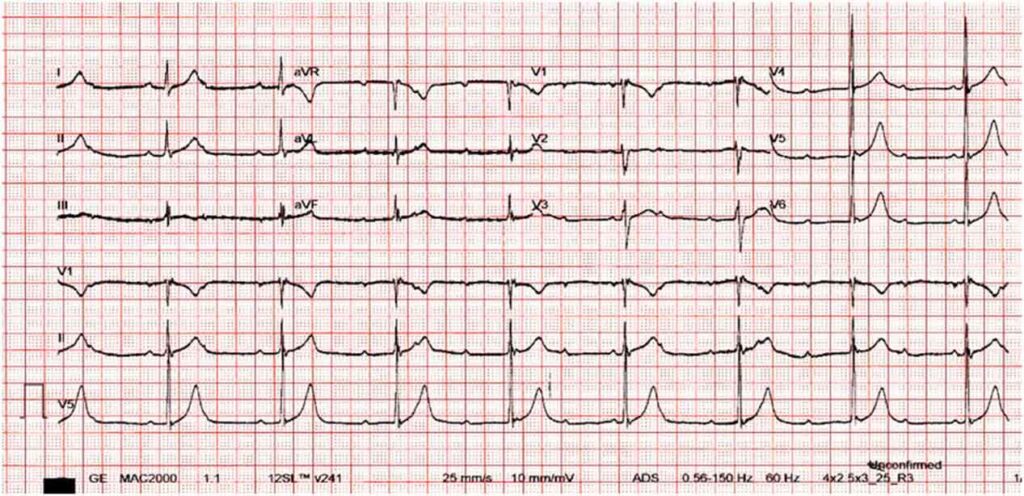
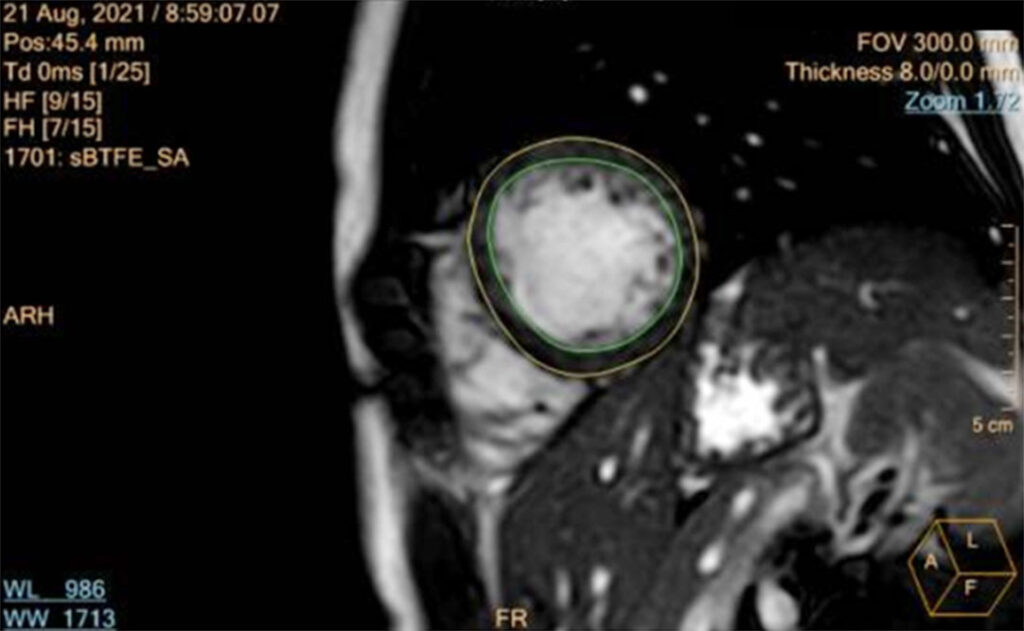
He was treated as a case of COVID Myocarditis, and was started on Intravenous Immunoglobulin infusion. However, despite completion of the immunomodulator, inotropic support and strict activity restriction, the patient continued to have hypotensive episodes, now with associated bradycardia. Repeat ECG was consistent with a High Grade Atrioventricular Block (Figure 2). A cardiac MRI was facilitated revealing a normal left ventricular cavity with preserved systolic function, with regional increase in T1/T2 signals matched with elevated ECV and subepicardial to midmyocardial hazy LGE at the septal wall to consider subacute myocarditis, and normal right ventricle with preserved systolic function. (Figure 3).
The patient, then, underwent insertion of the VVIr (ventricular demand with rate response) endovenus pacemaker and tolerated the procedure well with no intraoperative complications. He had a total blood loss of 5ml, and was later noted to have stable vital signs postoperatively. His BP was stable at 109-124/42-62mmHg, a HR or 76-90 bpm, O2 saturation of 100% at room air. Epinephrine was tapered and eventually discontinued. The patient remained stable for the remainder of this hospital stay (Figure 4). Repeat Chest X-ray done prior to discharge showed good pacemaker placement and interval resolution of the respiratory infiltrates. The patient was, then, discharged stable and improved.
DISCUSSION
Myocarditis is inflammation of the heart without an ischemic cause. Of patients infected with COVID 19, only 8-28% of adults present with myocardial involvement.2 The percentage of pediatric patients presenting with myocarditis has not been fully studied, however since younger patients tend to have milder symptoms, cardiac involvement and progression to fulminant organ failure is rare.
Viral infections have been identified as one of the most common causes of myocarditis, and since the onset of the pandemic, there have been reported cases of myocarditis secondary to the COVID 19 virus.3
Typically, cardiac injury from COVID 19 can range from a mild troponin leak to fulminant myocarditis. The pathophysiology of myocarditis secondary to COVID 19 is not well understood, however it is postulated to be related to the Angiotensin converting enzyme 2 (ACE2) expression in the heart tissue. ACE2 has previously been identified as a functional receptor for the COVID 19 virus, and this receptor has high expression in the lung, heart, endothelial cells, ileum and kidney. It is also because of this pathology that children are less susceptible to severe COVID 19 infection since ACE2 receptors are known to be more abundantly expressed on well differentiated ciliated epithelial cells. Once attached to the receptor, they induce chemoattractants that result in the infiltration of a large number of inflammatory cells, which induce direct injury to the affected organ.4 At present, arrhythmia is recognized to be one of the possible clinical manifestations in COVID myocarditis. This is said to be secondary to inflammation and edema of the conduction tissue as part of the global myocardial injury process.1
Cardiac arrhythmias are reported in 16.7% of hospitalized patients in a Chinese cohort study in Wuhan, China, but the exact nature of these arrhythmias were not well documented or published.5 Therefore, the prevalence of COVID 19 related arrhythmias still remains unknown. There was only 1 documented case of a patient with high-grade AV block secondary to COVID 19 seen in a 53 year old man, however this severe complication has not been previously seen in pediatric patients.3 Myocarditis, however, in rare cases, may lead to deterioration of cardiac function and subsequent cardiogenic shock.9
Suggested workup for patients with COVID 19 usually show elevated inflammatory markers (C-reactive protein, erythrocyte sedimentation rate, and lactate), which are consistent with the ongoing infection. However, further testing is recommended for patients with myocarditis, which includes N-terminal pro-B type natriuretic peptide, cardiac troponin T, and cardiac troponin I). This patient had regular monitoring of NT-proBNP and Troponin T levels over the course of the admission, which were consistent with the ongoing heart damage secondary to the virus. The American Heart Association also recommends cardiac imaging for patients with myocarditis, which can be but is not limited to an echocardiogram and/or a cardiac MRI, of which, our patient underwent both.
As in other cases of myocarditis secondary to a virus, the mainstay of treatment is maintaining hemodynamic stability with mechanical ventilation and intravenous inotropic support. The initiation of immunomodulatory therapy with IVIG and glucocorticoids still remains to be controversial. However with the patient’s ongoing COVID 19 infection, both IVIG and glucocorticoids were considered since they have demonstrated clinical efficacy on critically ill patients.6, 7 The IL-6 receptor monoclonal antibody, Tocilizumab, was also used in this patient’s treatment. Studies have shown that this antibody might be beneficial in the setting of cytokine storm syndrome, as seen with this patient’s elevated inflammatory markers, and subsequently help reduce myocardial infarction.
Finally, the management of the arrhythmia is still crucial in the final prognosis of this patient. A bradyarrhythmia, as was seen in this patient’s case, may require cardiac pacing. Third-degree AV block has been identified as one of the most common indications for pacemaker implantation in children,8 and given the patient’s age, response to treatment, and predicted course of improvement, a permanent pacemaker was inserted. Post-pacemaker implantation complications can include but are not limited to pneumothorax, hematoma, endocarditis/pericarditis, and surgical infection, hence close monitoring and follow up must be advised for the patient.
CONCLUSION
Although cardiac involvement in COVID 19 infection is rare in both adults and pediatric patients alike, the possibility of a fulminant myocarditis with resultant High Grade AV Block is possible. Because of this, patients with cardiac symptoms, persistent need for inotropic support and largely elevated cardiac markers must be closely monitored for more severe cardiac complications following a COVID 19 infection.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author Contributions
The authors confirm contribution to the paper as follows: case report conception: J.J.D.R.; draft manuscript preparation: P.M.R.; review and editing: J.J.D.R., J.A.N. All others reviewed the report and approved the final version of the manuscript.
Conflicts of interest
The authors declare that is no conflict of interest that may arise from the submission and publication of this manuscript.
REFERENCES
1. Siripanthong, B., Nazarian, S., Muser, D., Deo, R., Santangeli, P., Khanji, M. Y., Cooper, L. T., Jr, & Chahal, C. (2020). Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart rhythm, 17(9), 1463–1471. https://doi.org/10.1016/j.hrthm.2020.05.001\ CrossRef Pubmed
2. El-Assaad I, Hood-Pishchany MI, Kheir J, Mistry K, Dixit A, Halyabar O, Mah DY, Meyer-Macaulay C, Cheng H. Complete Heart Block, Severe Ventricular Dysfunction, and Myocardial Inflammation in a Child With COVID-19 Infection. JACC Case Rep. 2020 Jul 15;2(9):1351-1355. doi: 10.1016/j.jaccas.2020.05.023. Epub 2020 May 19. PMID: 32835278; PMCID: PMC7237189. CrossRef Pubmed
3. Ashok, V., & Loke, W. I. (2020). Case report: high-grade atrioventricular block in suspected COVID-19 myocarditis. European heart journal. Case reports, 4(FI1), 1–6. https://doi.org/10.1093/ehjcr/ytaa248 CrossRef Pubmed
4. Yuki, K., Fujiogi, M., & Koutsogiannaki, S. (2020). COVID-19 pathophysiology: A review. Clinical immunology (Orlando, Fla.), 215, 108427. https://doi.org/10.1016/j.clim.2020.108427 CrossRef Pubmed
5. Wang, D., Hu, B., Hu, C., Zhu, F., Liu, X., Zhang, J., Wang, B., Xiang, H., Cheng, Z., Xiong, Y., Zhao, Y., Li, Y., Wang, X., & Peng, Z. (2020). Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA, 323(11), 1061–1069. https:// doi.org/10.1001/jama.2020.1585 CrossRef Pubmed
6. Xiang, H. R., Cheng, X., Li, Y., Luo, W. W., Zhang, Q. Z., & Peng, W. X. (2021). Efficacy of IVIG (intravenous immunoglobulin) for corona virus disease 2019 (COVID-19): A meta-analysis. International immunopharmacology, 96, 107732. https://doi.org/10.1016/j. intimp.2021.107732 CrossRef Pubmed
7. Ranjbar, K., Moghadami, M., Mirahmadizadeh, A. et al. Methylprednisolone or dexamethasone, which one is superior corticosteroid in the treatment of hospitalized COVID-19 patients: a triple-blinded randomized controlled trial. BMC Infect Dis 21, 337 (2021). https://doi.org/10.1186/s12879-021-06045-3 CrossRef Pubmed
8. Suarez, K., & Banchs, J. E. (2019). A Review of Temporary Permanent Pacemakers and a Comparison with Conventional Temporary Pacemakers. The Journal of innovations in cardiac rhythm management, 10(5), 3652–3661. https://doi.org/10.19102/icrm.2019.100506 CrossRef Pubmed
9. Vaturi, M., Hasdai, D., Battler, A. (2002). Myocarditis and Cardiogenic Shock. In: Hasdai, D., Berger, P.B., Battler, A., Holmes, D.R. (eds) Cardiogenic Shock. Contemporary Cardiology. Humana Press, Totowa, NJ. https://doi.org/10.1007/978-1-59259-154-1_14
Copyright Information
