Case Report
August 2023, 32:2
First online: 21 August 2023
Case Report
Device Closure of Left Circumflex Coronary Artery to Coronary Sinus Fistula
Rajeev Bhardwaj, Professor & Head, MD, DM (Cardiology),1 Sanjeev Asotra, Associate Professor, MD, DM (Cardiology) 1
2 Department of Cardiology, Indira Gandhi Medical College, Shimla. (India).
Main author: Rajeev Bhardwaj. Set no 11, I block MMIMSR, Mullana, Ambala (India)133207.
Email: rajeevbhardwaj_dr@yahoo.com.
Mobile no.: +919418136300
ABSTRACT
A coronary artery fistula (CAF) is defined as a direct connection between a coronary artery with right heart chambers including the right atrium, right ventricle, coronary sinus, superior vena cava, or pulmonary arteries. Elective closure of coronary artery fistula by surgery or percutaneous transcatheter technique is generally accepted in the presence of symptoms. We report a case of successful percutaneous transcatheter device closure of coronary fistula, originating from the circumflex artery and draining into the coronary sinus. Key wordscoronary arteriovenous fistula, device closure, Amplatzer vascular plug
CASE
8 years female child presented with history of (H/O) palpitation since childhood. Palpitation was present at rest but increased on exertion. She also had precordial chest pain, which occurred on exertion and was relieved at rest within two to three minutes. There was no H/O breathlessness, no pedal oedema or neck pulsations. There was no past history suggestive of rheumatic fever. On examination, apex beat was in mid clavicular line in 5th intercostal space. Heart sounds were normal. There was grade 2 continuous in left lower parasternal area.
X Ray of chest showed mild cardiomegaly with cardio thoracic ratio of 55%. ECG showed T wave inversion in leads V1 to V3.
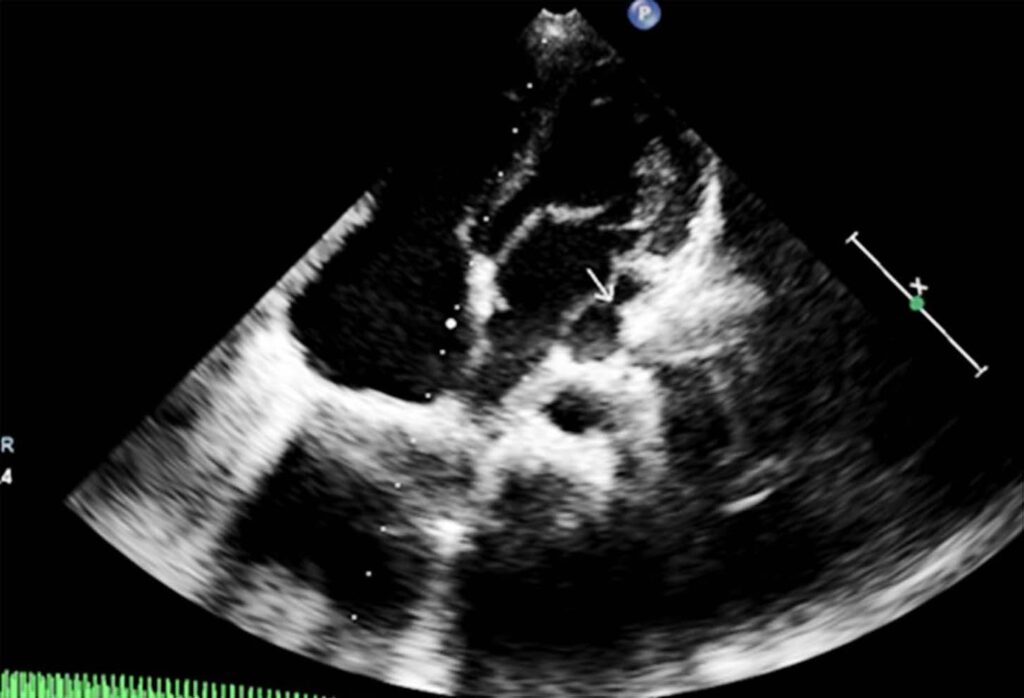
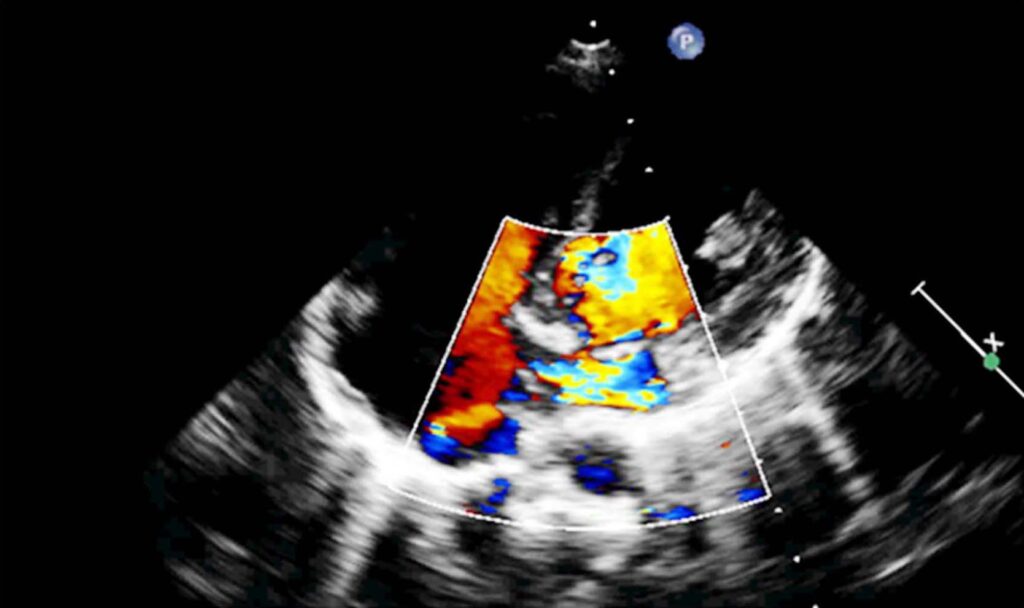
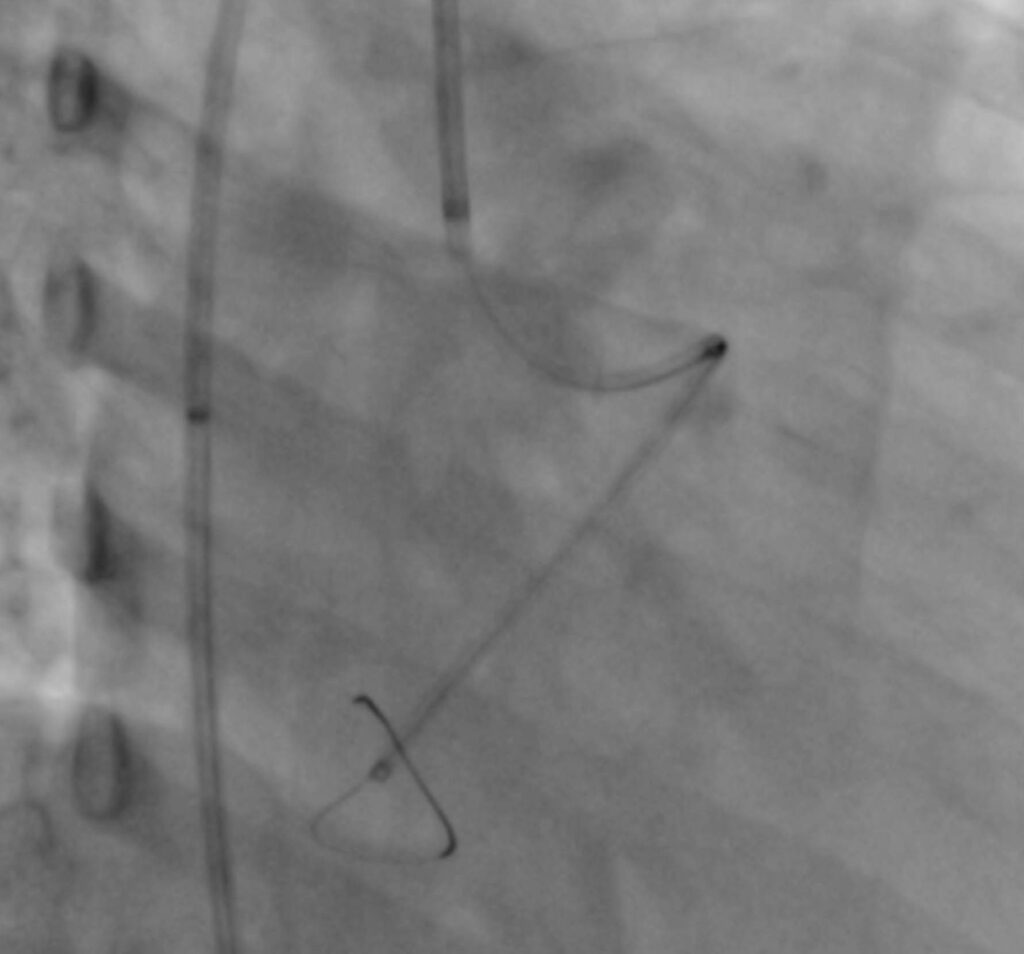
Echocardiography showed mild enlargement of right atrium and right ventricle. Coronary sinus was dilated (Figure 1). On colour Doppler, there were continuous signals in the coronary sinus (Figure 2). Coronary angiography was done, which showed normal right coronary artery. Left main coronary artery and left circumflex (LCX) were aneurysmally dilated and there was evidence of coronary artery fistula (CAF) between LCX and coronary sinus (CS). Left anterior descending (LAD) coronary artery was small due to low flow (Figure 3). MDCT was done, which showed size of communication as 5.3mm.

Patient was taken for device closure of fistula, in view of symptomatic status of the child. Initially we used Judkin,s left 3.0 guiding catheter, passed Amplatzer .035 guide wire into the LCX, but guiding catheter could not be negotiated. We now used Amplatzer (AL1) catheter. Again, passed Amplatzer guide wire.
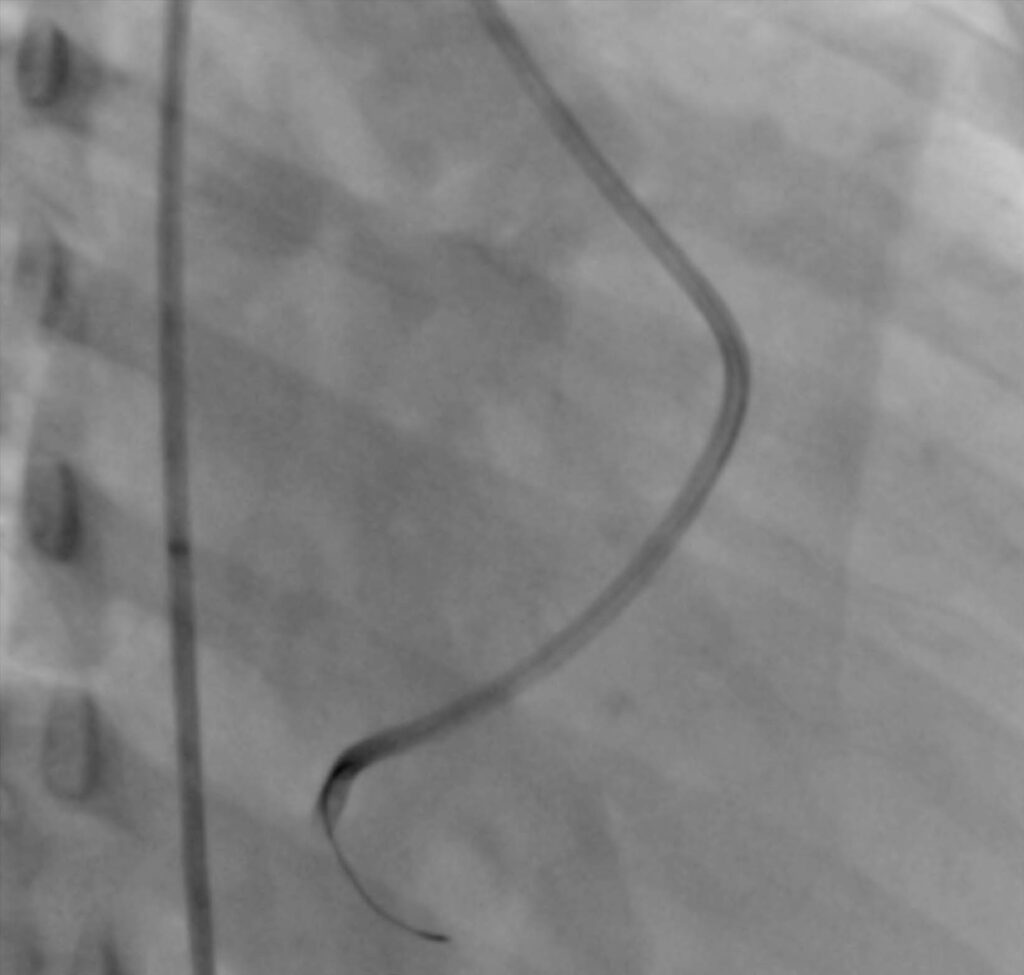
But due to obtuse angle of origin of LCX, guiding catheter could again not be negotiated. Even, use of another wire for support did not help. So, we passed BMW .014 guide wire into the distal LCX and passed GuideLiner (GL) over it (Figure 4). Now we could negotiate guiding catheter into the distal LCX over the GL (Figure 5). GL was then removed and 8 mm Amplatzer vascular plug was deployed, closing the defect (Figure 6). Complete closure was achieved (Figure 7). Patient was discharged next day on single antiplatelet. On three years follow up, patient is asymptomatic.
DISCUSSION
Krause et al first described CAFs in 1865.1 Coronary artery fistulas (CAF) are rare, their incidence is about 0.1–0.2% of congenital heart diseases.2 The majority of the CAFs are congenital in origin and usually involve the left anterior descending (LAD) artery (49%), right coronary artery (RCA) (33%), or less often the circumflex artery (17%). Congenital CAFs commonly drain to the right cardiac chambers or pulmonary circulation.3 The left circumflex coronary artery fistula communicating to the coronary sinus is rare.4 Coronary fistulas lead to steal of blood from the coronary artery to the low pressure cardiac chamber or vein causing ischemia distal to the site of the fistula.5 Moreover, decrease of coronary perfusion pressure due to distal run off will compensate over time by progressive dilatation of the fistulous tract that may lead to aneurysm formation and thrombosis.6 Sometimes patients with CAF present with high cardiac output congestive heart failure. These pathophysiological effects depend mainly on the size of the fistulous communication.
Surgical ligation is a safe and effective method however, postoperative care is longer and more complicated compared with a percutaneous closure.6 Transcatheter occlusion of a CAF was first reported in 1983. Many different types of occluding device have been used, including detachable balloons, Gianturco and other types of coils, Rashkind and Amplatzer duct occluder (ADO), and Amplatzer muscular ventricular septal defect devices, and vascular plugs. ADO has several advantages over other devices used to close CAF, such as the use of a single device, a high rate of complete occlusion, and improved control over the placement and release of the device. Percutaneous device closure of CAFs is usually a complex procedure taking a long procedural and fluoroscopy time. Not all coronary fistulas are amenable to percutaneous closure due to anatomic reasons. Mavroudis et al7 suggested some guidelines for anatomic characteristics allowing percutaneous closure of a CAF:
-
1. The ability to cannulate safely the branch coronary artery
that supplies the fistula;
- 2. Absence of large branch vessels that can be inadvertently embolized;
- 3. The presence of a single, narrow restrictive drainage site into the cardiac chamber or vessel; and
- 4. The absence of multiple fistulous communications.
We conclude that fistulous communication between LCX artery and CS is a rare cardiac anomaly that may present only with cardiac murmurs or features of volume overload or coronary steal. Our patient had features of both volume overload and coronary steal. It was difficult to close as LCX had very obtuse origin. We had to take the help of GL to negotiate the guiding catheter.
Conflict: None of the authors have any conflict of interest
REFERENCES
1. Kirklin JW, Barratt-Boyes BG. Congenital anomalies of the coronary
arteries. In: Kirklin JW, Barratt-Boyes BG. Cardiac Surgery. Third edition. New York, NY: Churchill Livingston; 1986: pp. 945-955.
2. V. Gupta, Q.A. Truong, D.R. Okada, T.J. Kiernan, B.P. Yan, R.J. Cubeddu, D.J. Roberts, S. Abbara, T.E. MacGillivray, I.F. Palacios. Giant left circumflex coronary artery aneurysm with arteriovenous fistula to the coronary sinus. Circulation, 118 (2008), pp. 2304-2307. CrossRef
3. Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Catheter Cardiovasc Diagn. 1990;21(1):28-40. CossRef Pubmed
4. Said SA, van der Werf T. Dutch survey of coronary artery fistulas in adults: congenital solitary fistulas. Int J Cardiol. 2006;106(3):323-332. CrossRef Pubmed
5. M.H. Yeon, Y.R. Choi, S.Y. Lee, J.W. Bae, K.K. Hwang, D.W. Kim, M.C. Cho, S.M. Kim. A rare combination of the left circumflex coronary artery fistula connecting a dilated coronary sinus with persistent left superior vena cava and multiple arteriovenous fistulae. Korean Circ J, 43 (2013), pp. 356-359. CrossRef Pubmed
6. T. Watanabe, M. Saotome, A. Kumazawa, T. Urushida, H. Katoh, H. Satoh, H. Terada, K. Yamashita, N. Shiva, H. Hayashi. Giant and aneurysmal left circumflex coronary fistula to coronary sinus—cardiovascular computed tomography imaging before and after surgical operation JC Cases, 5 (2012), pp. e96-e99. CrossRef Pubmed
7. Mavroudis C, Backer CL, Rocchini AP, Muster AJ, Gevitz M. Coronary artery fistulas in infants and children: a surgical review and discussion of coil embolization. Ann Thorac Surg. 1997;63(5):1235-1242. CrossRef Pubmed
Copyright Information
