Case Report
August 2023, 32:3
First online: 21 August 2023
Case Report
Case of An Isolated Tricuspid Valve Regurgitation Presenting as Right Sided Heart Failure
MM Cheng-Co,1* RM Rivera, 1* M Alegre,* S Sawit,1* G Martinez*
Email address of main and corresponding author: mmchengmd@gmail.com
ABSTRACT
Trivial to mild tricuspid regurgitation is commonly seen in patients with a normal right heart. It is usually asymptomatic and when severe enough may cause symptoms of right-sided heart failure such as ascites, edema and congestive hepatopathy. We present a case of a 46-year-old female who presented with progressive bipedal edema. Transthoracic echocardiography showed dilated right atrium and right ventricle with severe tricuspid regurgitation. Patient then underwent tricuspid valve replacement with a 29mm bioprosthetic valve. Final histopath report showed myxomatous degeneration of valve leaflets. Post-operatively, patient developed increasing shortness of breath and orthopnea. A repeat transthoracic echo revealed decompensation of right ventricle with decline in right ventricular systolic function. Patient was then given inotropic support with milrinone and norepinephrine and adequate diuresis with IV furosemide. She was gradually weaned off the inotropes. Prior to discharge, a repeat transthoracic echocardiogram done showed improvement of right ventricular systolic function and she was discharged on oral furosemide and spironolactone.
Keywords
Isolated tricuspid regurgitation, myxomatous valve, right-sided heart failure
INTRODUCTION
Trivial to mild tricuspid regurgitation is commonly seen in echocardiography of patients with a normal right heart. Causes of tricuspid regurgitation may be primary from an intrinsic valve defect such as rheumatic heart disease, Eibstein anomaly or prolapse from myxomatous valve changes. Tricuspid regurgitation is generally well tolerated and mostly asymptomatic. Symptoms of tricuspid regurgitation are predominantly related to right-sided heart failure such as ascites, edema and congestive hepatopathy. Tricuspid regurgitation when severe, may be considered for surgical replacement.
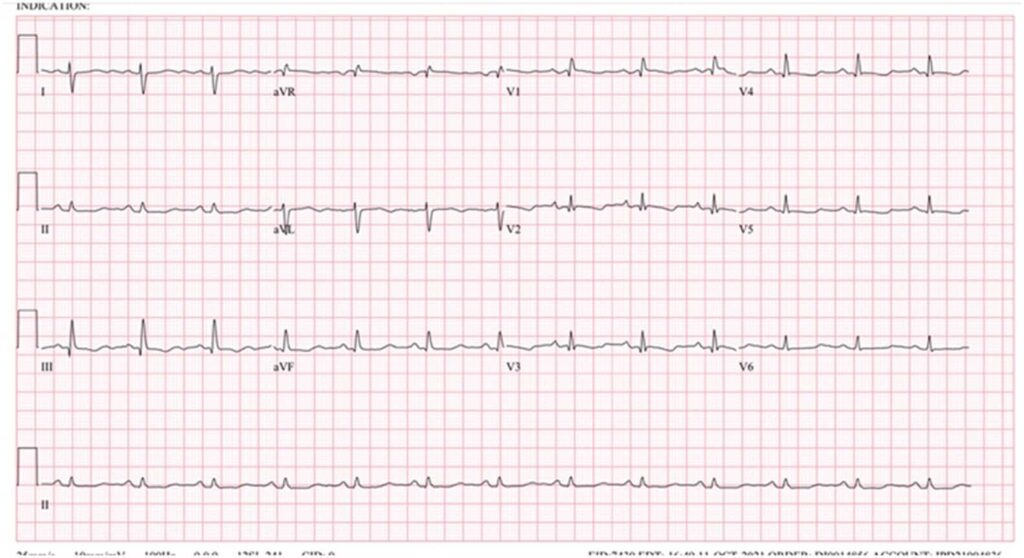
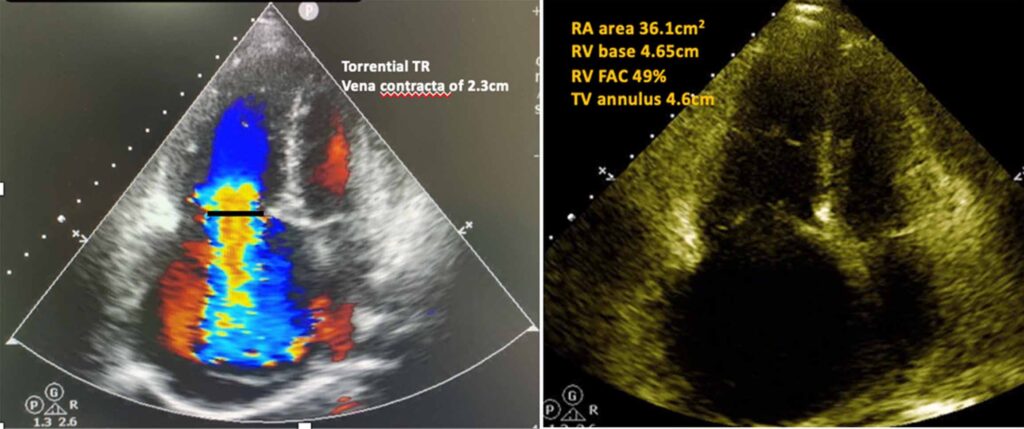
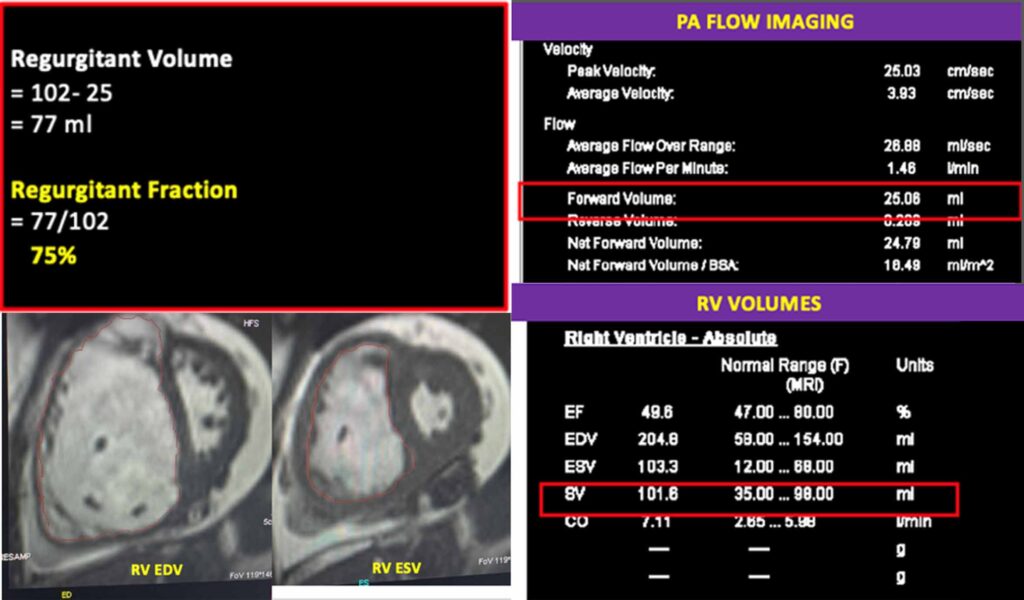
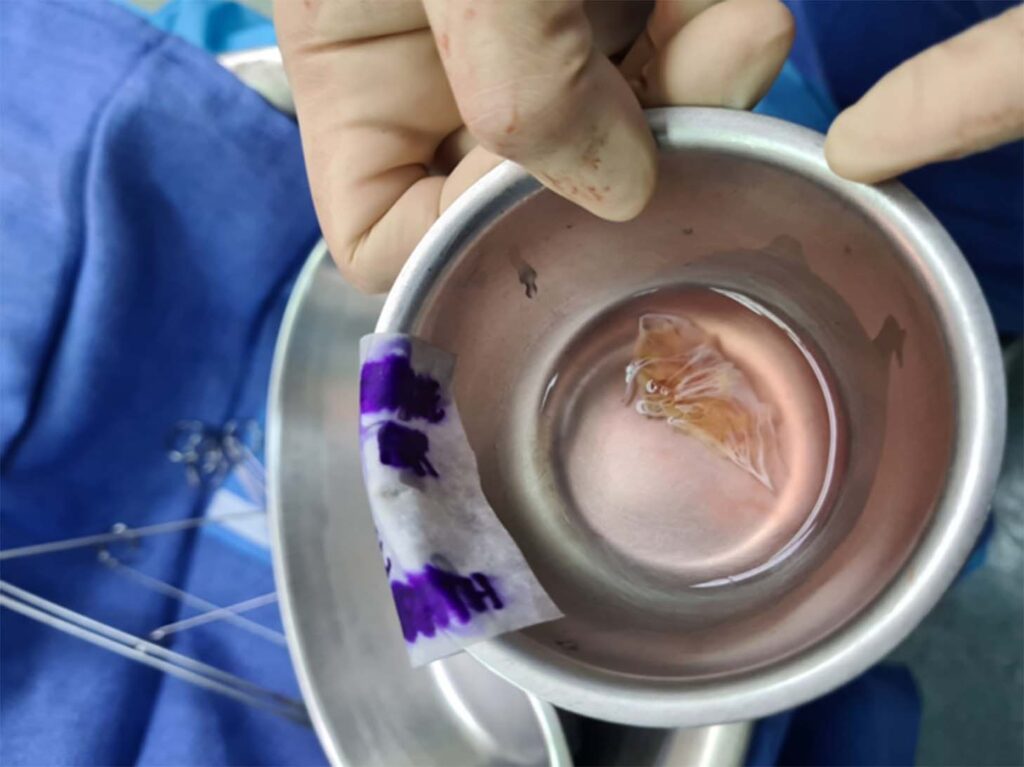
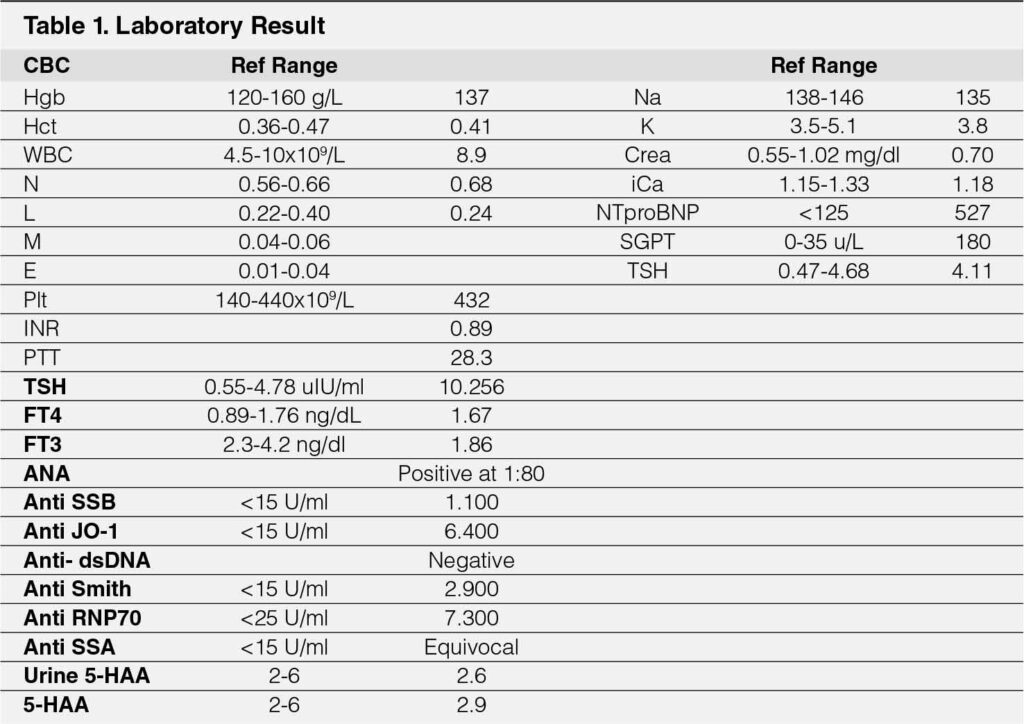
A 46-year-old female with no known comorbidities presented with 8 months duration of progressive bipedal edema. It was not accompanied by other signs of heart failure such as orthopnea, paroxysmal nocturnal dyspnea or exertional dyspnea. She initially sought consult with an internist and was given Furosemide on an as needed basis which helped relieve the edema. A month prior to admission, patient then noted persistence of edema despite daily intake of furosemide. At the time of admission, patient already had icteric sclerae, clear breath sounds, grade 4/6 systolic murmur loudest on 4th ICS, augmented by inspiration, with presence of RV heave and bipedal edema. Her 12L ECG showed sinus rhythm, right ventricular hypertrophy with QT prolongation (Figure 1). A transthoracic echocardiogram was then done which revealed dilated right ventricle with RV base of 4.7cm, dilated right atrium with right atrial area of 26.5cm2 and severe tricuspid regurgitation with DTI of 11cm/s, severe torrential regurgitation with vena contracta of 2.3cm (Figure 2). Right ventricular systolic function was normal with RV Fractional Area of Change (FAC) of 51.3% and TAPSE of 2cm. Cardiac MRI was done to investigate for other possible etiologies of the tricuspid regurgitation and to evaluate the right ventricular size and function. Cardiac MRI showed markedly dilated right ventricle with normal systolic function, enhancement of right ventricular insertion points which may be seen in right ventricular overload, dilated tricuspid valve annulus at 4cm and torrential tricuspid regurgitation with regurgitant volume of 77ml and regurgitant fraction of 75% (see Figure 3). Autoimmune work up was also done to rule out secondary causes of tricuspid regurgitation (see Table 1). Preoperative left and right heart catheterization was done which showed ventricularized c-v wave, attenuated x descent and rapid downstroke of y wave, elevated right sided pressures, pulmonary artery systolic pressure of 39.26mmHg, right ventricle pressure of 43/33mmHg and right atrial pressure of 43/32mmHg. Patient then underwent tricuspid valve replacement with a 29mm bioprosthetic valve. Intra-operatively, patient was noted to have dilated tricuspid valve annulus, retracted septal leaflet and part of anterior leaflet near anteroseptal commissure, chordae tendinae and leaflet were not thickened (see Figure 4). Final histopathology report showed myxomatous degeneration of valve leaflets. Post-operatively, patient developed increasing shortness of breath and orthopnea, with episodes of hypotension. A transthoracic echo was then done which revealed decompensation of the right ventricular systolic function with RV FAC now at 16% from previous of 49.3% but noted decrease in right atrial and ventricular size. Patient was then started on inotropic support with norepinephrine and milrinone. Adequate diuresis was also done with furosemide and spironolactone. Patient was then gradually weaned off from inotropes and maintained on oral diuresis with furosemide and spironolactone. Prior to discharge, a repeat 2D echo was done which showed slight improvement of right ventricular systolic function and presence of pericardial effusion. Colchicine was then added to home meds for the pericardial effusion.
DISCUSSION
Tricuspid valve regurgitation may be primary from a valve defect or most commonly functional and secondary from a mitral valve pathology. Isolated tricuspid valve regurgitation is rare. It is usually well-tolerated and often clinically unsuspected. Patients would usually come in for consult once heart failure symptoms have already set in. For asymptomatic patients, right ventricular size and function must be monitored as it is associated with poor survival outcomes and thus may be considered for early surgical intervention. Current management guidelines are directed towards underlying disease process and tricuspid valve replacement is recommended only for severe symptoms and as such, most of the current recommendations that we have for tricuspid valve surgery are targeted for patients with concomitant aortic and mitral valve replacement.1 Data is still lacking regarding outcomes of isolated tricuspid valve replacement due to its rarity. A high morbidity and mortality is associated with isolated tricuspid valve replacement in part due the development of right ventricular dysfunction. Right ventricular dysfunction after cardiac surgery is rare and is most commonly noted with tricuspid regurgitation correction. With correction of tricuspid regurgitation, there is development of right ventricular decompensation whenever the right ventricle cannot sustain the pressure and volume overload that occurs after the correction.2 With right ventricular dysfunction, careful consideration must be given to volume status by ensuring adequate diuresis. Factors that may also increase afterload such as hypoxia, acidosis and hypercapnia must be avoided and immediately addressed if present. Inotropes such as milrinone may be given to improve myocyte function and restore blood flow in tissues.3 Transcatheter therapies may have a role given that patients who undergo isolated tricuspid surgical valve replacement have high perioperative morbidity and mortality. However, given that our patient already has significant annular dilatation, she may not be an ideal candidate and surgical replacement may offer a better outcome. Studies are still emerging as to what subset of patients would benefit transcatheter tricuspid valve replacement.4
REFERENCES
1. Fender, E. A., Zack, C. J., & Nishimura, R. A. (2017). Isolated tricuspid
regurgitation: Outcomes and therapeutic interventions. Heart, 104(10),
798–806. https://doi.org/10.1136/heartjnl-2017-311586 CrossRef Pubmed
2. Cheng, Y., Mo, S., Wang, K., Fan, R., Liu, Y., Li, S., Zhang, X., Yin, S.,
Xu, Y., Tang, B., & Wu, Z. (2020). Mid-term outcome after tricuspid valve
replacement. Brazilian Journal of Cardiovascular Surgery, 35(5). https://doi.org/10.21470/1678-9741-2019-0215 CrossRef Pubmed
3. Levy, D., Laghlam, D., Estagnasie, P., Brusset, A., Squara, P., & Nguyen,
L. S. (2021). Post-operative right ventricular failure after cardiac surgery: A
cohort study. Frontiers in Cardiovascular Medicine, 8. https://doi.org/10.3389/fcvm.2021.667328 CrossRef Pubmed
4. Demir, O. M., Regazzoli, D., Mangieri, A., Ancona, M. B., Mitomo, S., Weisz, G., Colombo, A., & Latib, A. (2018). Transcatheter tricuspid valve replacement: Principles and design. Frontiers in Cardiovascular Medicine, 5.
https://doi.org/10.3389/fcvm.2018.00129 CrossRef Pubmed
Copyright Information
